FREE PDF new guidelines TCCC 24 Jan 2024 https://emssolutionsint.blogspot.com/2012/01/tactical-combat-casualty-care-tccc.html
A more careful and comparative reading with the previous edition will however allow some to note more profound modifications among others on the I-Gel.
DESCARGAR Guía 2024 #DrRamonReyesMD #CoTCCC #TCCC #Igel
Pues 4 años más. Instructor/Faculty/Medical Director TCCC-NAEMT Tactical Combat Casualty Care by Dr. Ramon Reyes, MD ∞🧩 𓃗https://emssolutionsint.blogspot.com/2012/01/tactical-combat-casualty-care-tccc.html TCCC Guidelines by JTS / CoTCCC. FREE pdf / Manual TCCC Español. FREE pdf. Updated TCCC Guidelines Guías " Tactical Combat Casualty Care English/Español #DrRamonReyesMD ∞🧩 @DrRamonReyesMD
#TCCC #CoTCCC #Medic #Tactical
Tactical Combat Casualty Care (TCCC)
Guidelines for Medical Personnel
05 November 2020
This is the Military Health System (Sistema de Emergencias del Ejercito de EUA) by Miliatary Health
Current Tactical Combat Casualty Care (TCCC) Guidelines as of 05 NOVEMBER 2020. The TCCC Guidelines are the standard of care for the modern battlefield. The guidelines cover: Care Under Fire (CUF), Tactical Field Care (TFC), Tactical Evacuation Care (TACEVAC). These recommendations are intended to be guidelines only and are not a substitute for clinical judgment. The Joint Trauma System (JTS) is focused on the standard of care for prehospital battlefield medicine. The JTS is a Department of Defense, Center of Excellence for Trauma providing clinical practice guidelines and performance improvement for all levels of military trauma care. The Committee on Tactical Combat Casualty Care (CoTCCC) is a committee of representatives from across the Army. Navy, Air Force and Marines positioned under the JTS that establishes clinical practice guidelines for the delivery of tactical combat casualty care (TCCC) on the battlefield. This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License. For more information, please visit https://creativecommons.org/.

Current Tactical Combat Casualty Care (TCCC) Guidelines as of 01 AUGUST 2019. The TCCC Guidelines are the standard of care for the modern battlefield.
The guidelines cover: Care Under Fire (CUF), Tactical Field Care (TFC), Tactical Evacuation Care (TACEVAC). These recommendations are intended to be guidelines only and are not a substitute for clinical judgment.
The Joint Trauma System (JTS) is focused on the standard of care for prehospital battlefield medicine. The JTS is a Department of Defense, Center of Excellence for Trauma providing clinical practice guidelines and performance improvement for all levels of military trauma care. The Committee on Tactical Combat Casualty Care (CoTCCC) is a committee of representatives from across the Army. Navy, Air Force and Marines positioned under the JTS that establishes clinical practice guidelines for the delivery of tactical combat casualty care (TCCC) on the battlefield.
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License. For more information, please visit https://creativecommons.org/.
El DHA se encuentra revisando los Curriculums en 4 Cursos TCCC
TCCC-All Services Member
TCCC-Combat Life Saver
TCCC-Combat Medic Corpsman
TCCC-Combat Paramedic
Todos Documentos Tactical Combat Casualty Care TCCC / TECC / TACMED en ESPAÑOL
DESCARGAR
https://www.jsomonline.org/TCCCEsp.php
UPDATED TCCC GUIDELINES. http://bit.ly/TCCC-GL
Review and download the updated Tactical Combat Casualty Care Guidelines at https://www.deployedmedicine.com/market/11/content/40or on the Deployed Medicine mobile app.
Take a look at the 01 AUG 2019 guideline update.
New recommendations for the use of the iTClamp as a primary treatment modality, along with a CoTCCC-recommended hemostatic dressing and direct manual pressure (DMP), for hemorrhage control in craniomaxillofacial injuries and penetrating neck injuries with external hemorrhage.
Always find the latest TCCC training and education materials at the Deployed Medicine website or on the mobile app available for iTunes, Android, and Google devices.
#TCCC #TC3 #TacticalCombatCasualtyCare#CoTCCC #CPG #ClinicalPracticeGuidelines#Prehospital #CombatCasualtyCare#BattlefieldMedicine #CombatMedicine #Medic#Corpsman #Pararescue #DeployedMedicine#TensionPneumothorax #Guidelines
#TCCCGuidelines #CommitteeonTCCC #JTS#JointTraumaSystem #HemorrhageControl#BleedingControl #NeckWounds#craniomaxillofacial #craniomaxillofacialinjury#penetratingneckinjury #NeckInjury #iTClamp 


Tactical Combat Casualty Care TCCC, TC3 by CoTCCC.
DERECHOS DEL LOGO
TCCC Guidelines by JTS / CoTCCC
#TCCCGuidelines by #JTS / #CoTCCC #free #pdf
#Tactical #Combat #Casualty #Care #TCCC
Current Tactical Combat Casualty Care (TCCC) Guidelines as of 01 AUGUST 2018. The TCCC Guidelines are the standard of care for the modern battlefield.
The guidelines cover: Care Under Fire (CUF), Tactical Field Care (TFC), Tactical Evacuation Care (TACEVAC). These recommendations are intended to be guidelines only and are not a substitute for clinical judgment.
The Joint Trauma System (JTS) is focused on the standard of care for prehospital battlefield medicine. The JTS is a Department of Defense, Center of Excellence for Trauma providing clinical practice guidelines and performance improvement for all levels of military trauma care. The Committee on Tactical Combat Casualty Care (CoTCCC) is a committee of representatives from across the Army. Navy, Air Force and Marines positioned under the JTS that establishes clinical practice guidelines for the delivery of tactical combat casualty care (TCCC) on the battlefield.
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License. For more information, please visit https://creativecommons.org/.
Tactical Combat Casualty Care Logo 2008.
|
| Type of Work: | Visual Material |
|---|
| Registration Number / Date: | VAu000969890 / 2008-09-03 |
|---|
| Application Title: | Tactical Combat Casualty Care Logo 2008. |
|---|
| Title: | Tactical Combat Casualty Care Logo 2008. |
|---|
| Description: | Electronic file (eService) |
|---|
| Copyright Claimant: | Frank Butler. Address: 4575 Lavallet Lane, Pensacola, FL, 32504 |
|---|
| Date of Creation: | 2008 |
|---|
| Authorship on Application: | Frank Butler; Citizenship: United States. Authorship: 2-D artwork. |
|---|
| |
|---|
| Names: | Butler, Frank
ENLACE COMPROBACION DE REGISTRO
|
|---|
|
|
Tactical Combat Casualty Care Quick Reference Guide.
|
| Type of Work: | Entry not found. |
|---|
| Registration Number / Date: | TXu002046564 / 2017-05-10 |
|---|
| Application Title: | Tactical Combat Casualty Care Quick Reference Guide. |
|---|
| Title: | Tactical Combat Casualty Care Quick Reference Guide. |
|---|
| Description: | Electronic file (eService) |
|---|
| Copyright Claimant: | Harold R. Montgomery, 1968- . Address: 5118 Sanderling Ridge Drive, Lithia, FL, 33547, United States. |
|---|
| Date of Creation: | 2017 |
|---|
| Authorship on Application: | Harold R. Montgomery, 1968- ; Domicile: United States; Citizenship: United States. Authorship: text, artwork. |
|---|
| Rights and Permissions: | Harold R. Montgomery, 5118 Sanderling Ridge Drive, Lithia, FL, 33547, United States, (706) 464-3121, (706) 464-3121, hrmontgomery75@gmail.com |
|---|
| Copyright Note: | C.O. correspondence. |
|---|
| |
|---|
| Names: | Montgomery, Harold R., 1968-
https://cocatalog.loc.gov/cgi-bin/Pwebrecon.cgi?v1=9&ti=1,9&SAB1=tactical%20casualty%20care&BOOL1=all%20of%20these&FLD1=Keyword%20Anywhere%20%28GKEY%29%20%28GKEY%29&GRP1=OR%20with%20next%20set&SAB2=&BOOL2=as%20a%20phrase&FLD2=Keyword%20Anywhere%20%28GKEY%29%20%28GKEY%29&CNT=10&PID=zQyTB_2tQ-hS8fOn4jIJhlQYF22hD&SEQ=20190830051206&SID=14
|
|---|
Dr. Frank K. Butler CoTCCC Committee of Tactical Combat Casualty Care Chair. Receives the Distinguished Service Award for lifetime achievement
By: Military Health System Communications Office
Vice Admiral Raquel C. Bono, director of the Defense Health Agency, presented Frank K. Butler, Jr., M.D. with the 2017 Distinguished Service Award, in the category of Combat Casualty Care, today at the Military Health System (MHS) Research Symposium. The Distinguished Service Award is a lifetime achievement award recognizing an individual who contributed significantly to the success of MHS research and who demonstrates outstanding leadership.
According to his nomination, “Butler's name is synonymous with prehospital trauma care.” He facilitated, promoted, and applied the results of MHS research in his roles as a founder of Tactical Combat Casualty Care (TCCC) and director of the Prehospital Care Branch at the Joint Trauma System. His years of dedication and expertise led to multiple casualty care breakthroughs for military application that crossed into the civilian trauma care world. Butler's contributions to trauma care are immeasurable with world-wide acceptance and implementation.
Butler retired as a Captain from the U.S. Navy Medical Corps and is now a staff ophthalmologist for the Naval Hospital, Pensacola. He currently chairs the Committee on TCCC and serves as a medical consultant for the Navy Medical Lessons Learned Center.
Throughout his military career, Butler held many positions beginning with the Platoon Commander for SEAL Team One and the Underwater Demolition Team Twelve, culminating to the command surgeon for the U.S Special Operations Command. To learn more about his exciting career, please view
Frank K. Butler, Jr., MD PHTLS Consultant to the Committee on Military Medicine Email: Frank.Butler@med.navy.mil Frank K. Butler, Jr., MD, is retired as Captain, Medical Corps, U.S. Navy and is staff ophthalmologist for the Naval Hospital, Pensacola, Fla. He currently chairs the Committee on Tactical Combat Casualty Care and serves as a medical consultant for the Navy Medical Lessons Learned Center. He also serves as president of DSO Medical Consultants, LLC, and as a member of the board of the Undersea and Hyperbaric Medical Society. In addition to serving as a member of the PHTLS Executive Council, Butler is a member of the NOAA Diving Medical Review Board and an ophthalmology consultant for Diver’s Alert Network. Previously, Butler was command surgeon for the United States Special Operations Command; editor, Journal of Special Operations Medicine; and chair, USSOCOM Biomedical Initiatives Steering Committee. He served as a surgeon through the Joint Task Force Five in Afghanistan in 2003 and as Biomedical Research Director for Naval Special Warfare Command. He’s also worked as Chief of Ophthalmology, Naval Hospital Pensacola; Diving Medical Research Officer, Navy Experimental Diving Unit; Platoon Commander for SEAL Team One and Platoon Commander for Underwater Demolition Team Twelve. After attending the Georgia Institute of Technology and earning his M.D. from the Medical College of Georgia, Butler worked as an intern in family practice at the Navy Regional Medical Center, Jacksonville, Fla., from 1980-1981. He completed his ophthalmology residency at the National Naval Medical Center, Bethesda, Md., and served as chief resident, Undersea Medical Officer Training, Navy Undersea Medical Institute. Butler is a Fellow of the American Academy of Ophthalmology and a member of the Undersea and Hyperbaric Medical Society, Special Operations Medical Association, Association of Military Surgeons of the United States, American Medical Association and Wilderness Medical Society. He has published in more than 20 publications, textbooks and symposiums, including for the Undersea Medical Society, Ophthalmology, and the Annals of Surgery
UPDATED list of CoTCCC-Recommended Limb Tourniquets as of 06 MAY 2019.
Over the past year, the Committee on TCCC has conducted a comprehensive review of commercial limb tourniquets. After careful review using specific criteria, the recommended list of tourniquets is now available. The review criteria and specifics on each tourniquet will be published soon in medical literature.
Combat Application Tourniquet (CAT) Gen 7
NSN: 6515-01-521-7976
DLA Nomenclature: Tourniquet Nonpneumatic Combat Application One-Handed 37.5" LG 1
Combat Application Tourniquet (CAT) Gen 6
NSN: Use of CAT Generation 6 is acceptable until life-cycle replacements to gen 7.
DLA Nomenclature: Tourniquet Nonpneumatic Combat Application One-Handed 37.5" LG 1
Ratcheting Medical Tourniquet -Tactical (RMT-T)
NSN: 6515-01-527-3841
DLA Nomenclature: Tourniquet, One Handed Burke Device Tactical
NOTE: The RMT Civilian models are not CoTCCC-recommended for military use.
SAM Extremity Tourniquet (SAM-XT)
NSN: 6515-01-670-2240
DLA Nomenclature: Tourniquet Nonpneumatic 25S
SOF Tactical Tourniquet – Wide (SOFTT-W)
NSN: 6515-01-587-9943
DLA Nomenclature: Tourniquet Nonpneumatic Nylon Strap 1.5” Wide Nylon Strap for BR
NOTE: The original 1” SOFTT is removed from the CoTCCC Recommendations.
Tactical Mechanical Tourniquet (TMT)
NSN: 6515-01-656-6191
DLA Nomenclature: Tourniquet Nonpneumatic Tactical Mechanical Tourniquet
TX2” Tourniquet (TX2)
NSN: 6515-01-667-6027
DLA Nomenclature: Tourniquet Nonpneumatic TX2 Ratcheting One-Hand Coyote
TX3” Tourniquet (TX3)
NSN: 6515-01-667-6208
DLA Nomenclature: Tourniquet Nonpneumatic TX2 Ratcheting OD Green
PNEUMATIC LIMB TOURNIQUETS
Emergency Medical Tourniquet (EMT)
NSN: 6515-01-580-1645
DLA Nomenclature: Tourniquet Pneumatic Single-hand application fits upper and lower
NOTE: not recommended for JFAK, but considered for medics, evacuation platforms and Role I/II/III teams primarily for TQ-replacement, conversion, or prolonged application.
Tactical Pneumatic Tourniquet 2” (TPT2)
NSN: 6515-01-656-4831
DLA Nomenclature: Tourniquet Pneumatic Slide Fastener
NOTE: not recommended for JFAK, but considered for medics, evacuation platforms and Role I/II/III teams primarily for TQ-replacement, conversion, or prolonged application.
Joint Trauma System (JTS) / Committee on Tactical Combat Casualty Care (CoTCCC). The CoTCCC is the branch of the JTS focused on the standard of care for prehospital battlefield medicine. The JTS is the Department of Defense Center of Excellence for Trauma providing clinical practice guidelines and performance improvement for all levels of military trauma care.
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License. For more information, please visit https://creativecommons.org/.
#TCCC #TC3 #Tourniquet #CoTCCC #TacticalCombatCasualtyCare #CombatCasualtyCare
#CommitteeonTCCC #TourniquetRecommendations #LimbTourniquets #Tourniquets
#BattlefieldMedicine #Medic #Corpsman #Pararescue #CombatMedic #IFAK #JFAK
#NonpneumaticTourniquet
Law Enforcement and First Response Tactical Casualty Care (LEFR-TCC) to Tactical Combat Casualty Care for All Combatants (TCCC-AC).
Informacion importante sobre transicion de curso NAEMT:
06 de Junio 2017 Direccion NAEMT
El Curso Law Enforcement and First Response Tactical Casualty Care (LEFR-TCC) pasa en lo adelante a impartirse como Tactical Combat Casualty Care for All Combatants (TCCC-AC).
En Caso de tener alguna duda o requerir alguna aclaracion al respecto, puede comunicarse con su presentante local de la NAEMT o en su caso comunicarse directamente a las propias oficinas de la NAEMT en EUA al siguiente numero (Atentos hablan en Español)
NAEMT Headquarters at
National Association of Emergency Medical Technicians
Toll Free: 1-800-34-NAEMT
#NAEMT #TCCCAC #TCCLEFR #LEFRTECC#TacticalCourse #TCCC #CoTCCC
TACTICAL COMBACT CASUALTY CARE TCCC -
PREHOSPITAL TRAUMA LIFE SUPPORT - PHTLS - NAEMT - TCCC -TC3
El Material del Curso TCCC Tactical Combat Casualty Care es de acceso libre y gratuito, perteneciente CoTCCC Committee on Tactical Combat Casualty Care bajo el apoyo del Departamento de Defensa (DoD) de los Estados Unidos de America EUA
TCCC Faculty
TECC Director Pais y Facultado Internacional
Director Pais y Facultado Internacional PHTLS
The Committee on Tactical Combat Casualty Care (CoTCCC) is the
Prehospital arm of the Joint Trauma System for the Department of Defense.
The CoTCCC is composed of 42 voting members
specially selected as subject-matter experts in trauma, battlefield medicine,
tactical medicine, prehospital medicine and their experience in the deployed
combat environment. The TCCC Working Group is composed of the CoTCCC
and hundreds of subject-matter experts across many domains and liaisons from
DoD, Government and Partner nation organizations.
The CoTCCC and the TCCC Working Group focus all of
their efforts on providing the best recommendations for training and equipment
for our individual service members, combat medics, corpsman, pararescue, and
med techs going into harm’s way around the world.
El Comite de Tactical Combat Casualty Care (CoTCCC) es el brazo
prehospitalario del que se articula el
Sistema de Trauma del Departamento de Defensa de los EUA.
El CoTCCC está compuesto por 42 miembros votantes especialmente
seleccionados como expertos en materia
de trauma, medicina de combate, medicina táctica, medicina prehospitalaria y su
experiencia en despliegue en ambientes de combate. El Grupo de Trabajo del CoTCCC
está compuesto por cientos de expertos alrededor de dominios y alianzas desde
el DOD (Departamento de Defensa). Organizaciones del Gobierno y Organizaciones
Asociadas.
El CoTCCC y el Grupo de Trabajo del TCCC enfoca todo su esfuerzo en para proveer las mejores
recomendaciones para entrenamiento y equipamiento para nuestros miembros en
servicio de forma individual, Medic (Enfermero de Combate), Cuidador,
Pararescue (Especialista en Rescate de la Fuerza Aérea de Estados Unidos) y técnicos
médicos yendo dentro de la vía de los que han sufrido daño físico alrededor del
mundo
El Programa de
Formación Continuada Soporte Vital en el Trauma Prehospitalario
(PHTLS) se complace en presentar en nuestro país, el plan de formación
actualizado por el CoTCCC para el curso TCCC (Tactical Combat Casualty
Care).
El curso TCCC es un curso complementario al PHTLS
para los militares y los soldados que se están instruyendo para el
despliegue en operaciones de combate.
El curso PHTLS enseña los principios básicos para
el manejo del paciente traumatizado. El contenido de este programa
educativo enfatiza la necesidad de contar con un pensamiento crítico y
con una base consolidada de conocimientos para modificar la asistencia
al paciente dependiendo de la situación, el estado del paciente, los
conocimientos y la destreza del interviniente y de los recursos
disponibles en el momento en el que se necesita la asistencia. Estas
son las prioridades necesarias para aplicar correctamente los
principios de una buena asistencia al paciente - otra forma de ver la
“Ciencia y el Arte” del manejo del trauma.
En el entorno del combate, la situación es muy
diferente a la del entorno civil. La asistencia al herido en este
escenario debe ser la mejor combinación posible de una buena medicina y
de una buena táctica de las pequeñas unidades. Es fundamental que los
individuos posean las cualidades tanto tácticas como asistenciales en
cuidados médicos adecuadas. Los cuidados específicos en los escenarios
tácticos dependerán de la situación táctica, de las lesiones que
presente el herido, de los conocimientos y la destreza del primer
interviniente (el cuál puede no ser médico ni sanitario), y del equipo
médico que se tenga a mano.
 |
| “Con Armas, Casco, Chaleco antibalas y
uniforme. Pero en algo somos diferentes, nuestro objetivo. Salvar vidas
sin importanos quien sea” Dr. Ramon REYES, MD, EMT-T |
A diferencia de los escenarios de un Departamento
de Emergencias, dónde el paciente ES la misión, en el campo de batalla
la asistencia proporcionada a los heridos ES SOLO UNA PARTE de la
misión. El TCCC reconoce este hecho y estructura sus directrices para
conseguir tres metas prioritarias:
- Tratar al herido.
- Evitar heridos adicionales.
- Completar la misión.
En combate se producen muchos
cambios que afectan al cuidado del paciente. Aunque los principios
sobre el manejo del trauma pueden ser aplicados, las prioridades
asistenciales deben variar significativamente.
El programa TCCC , es un curso de tres días, que se ha creado para adaptar los principios de un buen manejo del trauma para su empleo exitoso en el campo de batalla.
La necesidad de un comité en TCCC que asegure que las directrices del TCCC son actualizadas y reflejan los nuevos avances en la medicina prehospitalaria y la experiencia en combate del TCCC se reflejó en el documento original del TCCC de 1996.
PHTLS reconoció la importancia del concepto TCCC en sus inicios y ha trabajado con el CoTCCC conjuntamente en los esfuerzos para darlo a conocer. El primer paso fue publicar el TCCC en el manual PHTLS. El siguiente paso ha sido crear una versión militar del manual PHTLS.
PHTLS se
complace en presentar el curso TCCC para el personal prehospitalario
militar y táctico-policial que lo necesite.
• Historia del Curso Tactical Combat Casualty Care (TCCC)
La atención al trauma prehospitalario en el combate varía en
muchos aspectos de la atención prehospitalaria al trauma que se practica
en el sector civil.
El personal médico de combate encara múltiples desafíos en la asistencia
de los miembros heridos de su equipo en entornos tácticos. Deben
proporcionar asistencia mientras se encuentran bajo fuego enemigo, a
menudo trabajando en la oscuridad con múltiples heridos y equipo
limitado. Deben también enfrentarse con tiempos prolongados de
evacuación. Los protocolos para el tratamiento desarrollados para los
entornos civiles no necesariamente se adaptan bien al campo de batalla.
Muertes prevenibles y heridos adicionales innecesarios se pueden
producir en el entorno táctico si no son considerados cuando se
desarrollan las estrategias de atención al trauma en combate.
La necesidad de reconsiderar la atención al trauma en el entorno
táctico ha sido ampliamente reconocida. , , El proyecto Tactical
Combat Casualty Care (TCCC) fue iniciado por El Mando de Guerra Naval
Especial (Naval Special Warfare Command) en 1993, y continuado
posteriormente por el Mando de Operaciones Especiales de Estados Unidos
(U.S. Special Operations Command (USSOCOM)). Este esfuerzo desarrolló un
conjunto de protocolos de atención al trauma en combate tácticamente
apropiados que fueron publicados como suplemento del manual de Medicina
Militar en 1996. Las directrices TCCC proporcionan a los médicos y
sanitarios en combate con estrategias de manejo del trauma una
combinación de buena medicina con buenas tácticas de las pequeñas
unidades.
Las directrices TCCC reconocen que la atención al trauma en el entorno táctico tiene tres objetivos:
1) tratar al herido
2) prevenir heridos adicionales
3) completar la misión.
Las medidas para la atención al trauma propuestas en las directrices originales del TCCC incluían:
• Una aproximación a la atención táctica del trauma en 3-fases
• Torniquetes
• Antibióticos de campaña
• Reanimación con fluidos tácticamente apropiada
• Mejora de la analgesia en combate (IV vs. Morfina IM)
• Vías aéreas nasofaríngeas como dispositivos de primera línea
• Vías aéreas quirúrgicas para traumas maxilofaciales con obstrucción de la vía aérea
• Diagnóstico y tratamiento agresivos del neumotórax a tensión
• Colaboración del Médico de Combate en la redacción de las directrices TCCC
• Entrenamiento basado en escenarios TCCC
• Combinación de buenas tácticas con Buena medicina
Como su nombre implica, el TCCC es praticado durante las misiones de
combate. La atención al trauma prehospitalario en lo militar es
comúnmente proporcionada por el siguiente personal médico de combate:
médicos del Ejército, sanitarios en la Armada y en los Marines, y
médicos y “PJ`s” (Pararescatadores) en la Fuerza Aérea.
El TCCC se divide en tres fases: Care Under Fire; Tactical Field Care;
Tactical Evacuation Care. En la fase Care Under Fire el personal medico
de combate y sus unidades se encuentran bajo fuego hostil efectivo y la
asistencia que pueden proporcionar es muy limitada. En la fase Tactical
Field Care, el personal médico y sus heridos no se encuentran bajo
fuego hostil efectivo, y puede proporcionarse un tratamiento más
extenso. En la fase de Tactical Evacuation Care, los heridos son
transportados a instalaciones médicas mediante una aeronave o un
vehículo terrestre, y se presenta la oportunidad de proporcionar
personal y equipamiento médico adicional para incrementar el nivel de
asistencia prestada.
El primer curso TCCC tuvo lugar en 1996 en la Oficina Médica Subacuática
patrocinado por la Oficina de Medicina y Cirugía Naval (BUMED). Poco
después, este entrenamiento fue obligatorio para todos los sanitarios
del SEAL . Desde entonces, ha ido ganado gradualmente aceptación en las
Fuerzas Armadas estadounidenses - y aliadas . También ha encontrado
aceptación en la comunidad médica civil de las fuerzas de seguridad .
La incorporación de las directrices del TCCC en el manual de
Soporte Vital al Trauma Prehospitalario (PHTLS) fué un importante
avance en el proceso de transición del TCCC. La cuarta edición de este
manual, publicado en 1999, contiene por vez primera un capitulo de
medicina militar15. Las recomendaciones contenidas en el manual PHTLS
llevan la aprobación del Comité del Trauma del Colegio Americano de
Cirujanos y de la Asociación Nacional de Técnicos en Emergencias. El
TCCC es el único conjunto de directrices de atención al trauma en
combate que ha recibido nunca este doble reconocimiento.
• El Comité del Tactical Combat Casualty Care
La necesidad de una
actualización periódica de las directrices del TCCC fue reconocida en
los comienzos en al desarrollarse el TCCC4. El documento original del
TCCC recomendaba que las directrices del TCCC sean actualizadas como
sea necesario por un comité del Departamento de Defensa creado a tal
efecto. Este concepto fue aprobado por el Mando de Operaciones
Especiales de los Estados Unidos, y el Comité del Tactical Combat
Casualty Care (CoTCCC) fue fundado posteriormente en 2001/2002 como
parte del proyecto de investigación biomédica del USSOCOM. El Mando
eligió ejecutar el proyecto, el Instituto de Medicina Operacional
Naval, posteriormente lo coordinó de manera extensa con los jefes de la
Medicina Naval para asegurarse de que sus esfuerzos llegarían a buen
término. El BUMED apoyó financieramente y con personal al CoTCCC en sus
inicios en el año fiscal de 2004. En los años fiscales 2007-2009, la
Oficina General de Cirugía del Ejército y el Instituto de
Investigaciones Quirúrgicas del Ejército estadounidense también
proporcionó apoyo al Comité.
El principio básico del TCCC consiste en proporcionar la mejor
asistencia médica posible combinada con buenas tácticas de las pequeñas
unidades, esto fue tan esencial que la lista de miembros del CoTCCC
incluye a personal médico de combate como a otros médicos. Esto también
es esencial para tener una representación de los tres Ejércitos para
asegurarse que las diferencias entre doctrina y experiencia de los
departamentos médicos del Ejército, la Armada, y la Fuerza Aérea son
reflejadas. Los médicos de combate seleccionados incluyen sanitarios del
SEAL de la Armada, sanitarios de la Armad asignados s unidades de
Marines, médicos Ranger, sargentos médicos de las Fuerzas Especiales,
PJ`s (Pararescatadores) de la Fuerza Aérea, aviadores médicos de la
Fuerza Aérea, y especialistas en sanidad de los Guardacostas. La lista
de miembros de otras especialidades incluye representaciones de cirugía
de trauma, medicina de emergencia, cuidados intensivos, y comunidades
de medicina operacional. También están representados los asistentes
médicos, planificadores médicos y educadores médicos.
En 2007, se vio
incrementado el protagonismo del TCCC en la Guerra Global Contra el
Terror (GWOT). El Mando de Apoyo de Medicina Naval propuso que el CoTCCC
fuese ascendido a un mando conjunto superior. Esta tarea fue encargada
a las oficinas de las Secretaría de Asistencia del Departamento de
Sanidad (ASD/HA) y al Cirujano para la Junta de Jefes de Personal. En
marzo de 2008. el CoTCCC fue recolocado para funcionar como una
subsecretaría del Consejo de Salud de la Defensa, el cuál tiene como
una de sus misiones el proporcionar consejos médicos a los tres
servicios de Cirugía General y a la ASD/HA.
• Actualizaciones TCCC 2003 y 2006
El CoTCCC ha continuado
controlando tanto los avances en medicina y tecnología como los cambios
en las técnicas y procedimientos de combate que se han ido produciendo
desde el 2001. Ha utilizado esta información para la actualización
continuada de las directrices del TCCC. Esto era inicialmente realizado
en ciclos de 3-4 años que coincidía con la publicación del manual
PHTLS. Actualmente se han dado cuenta de que las directrices deben ser
actualizadas básicamente con mayor frecuencia y de que las directrices
podrán también ser publicadas de forma más temprana usando la
tecnología basada en Internet.
El CoTCCC actualiza las directrices basándose en: 1) en la revisión
continua de las publicaciones de medicina prehospitalaria civiles y
militares; 2) en la interacción continua con los laboratorios militares
de investigación de atención a heridos en combate; 3) datos de primera
mano procedentes de sanitarios de combate, médicos, y PJ`s
experimentados; 4) opiniones de expertos tanto militares como civiles.
Las ediciones de 2003 y 2006 (quinta16 y sexta17) del Manual PHTLS
incorporan un número adicional de técnicas y tecnologías dentro de las
directrices del TCCC, incluyendo:
- Agentes Hemostáticos
- Dispositivos de infusion intraósea
- Paquete de Píldoras de Combate (antibióticos y analgésicos orales)
- Reanimación hipotensiva con Hextend
- Aplicadores de Fentanilo
- Prevención de la hipotermia
- Manejo de combatientes hostiles heridos
- 8 Reglas básicas para determinar las prioridades de evacuación
significativo de heridos iraquíes civiles y militares."18 La 101 División Aerotransportada cExperiencia en Combate con el TCCC en la Guerra
Un artículo en la “Punta de Lanza”, publicación oficial del Mando de Operaciones Especiales de Estados Unidos, afirma que: “Múltiples informes procedentes de Primeros Intervinientes de OE`s acreditan que las técnicas y el equipamiento TCCC están salvando vidas en el campo de batalla”20 El General Doug Brown, Comandante del USSOCOM, mandó una carta de agradecimiento al Cirujano General del Ejército por el excepcional trabajo realizado por el Instituto de Investigación Quirúrgica de Ejercito de los Estados Unidos (USAISR) en el establecimiento de un programa piloto llamado “Iniciativa de Transición” a una trayectoria rápida hacia un nuevo entrenamiento y equipamiento TCCC para desplegar unidades de OE`s y para recopilar datos acerca del éxito de estas medidas.Numerosos estudios publicados en la literatura médica y testimonios recogidos de los primeros intervinientes en combate han documentado que el TCCC está salvando vidas en el campo de batalla y está mejorando la continuidad táctica de las misiones en las que se produce el herido.
Tarpey describe el uso del TCCC por elementos de la Tercera División de Infantería en la fase inicial de la guerra en Iraq: “La adopción e implementación de los principios del TCCC por el pelotón médico de la Task Force 1-15 en OIF 1 resultan en un éxito arrollador. En más de 25 días de continuos combates con 32 bajas amigas, muchas de ellas graves, tuvimos 0 Muertos en Combate y 0 Muertos por Heridas, mientras tratábamos simultáneamente a un número
|
omprobó que “por la enseñanza y la utilización de ideas (TCCC), la 101 había alcanzado una de las tasa más elevadas de supervivencia en combate que ninguna otra unidad en el Ejército.” 19
|
Uno de los principales médicos
de la lista de la Unidad de Misiones Especiales del Ejército quién ha
tenido experiencia extensa en la utilización del TCCC parar el
tratamiento de heridos en combate, en una presentación a la Asociación
Médica de Operaciones Especiales en Diciembre de 2005, hizo la
siguiente recomendación: “Implementar el TCCC en todos los
entrenamientos de servicios médicos AHORA.” 6La carta del General Brown
afirma que el programa TCCC del USAIRS tuvo:”…produjo avances
reseñables en la habilidad de nuestra fuerza para el manejo exitoso del
trauma en combate.” 21 22
Un equipo del Centro Médico Militar empleó un entrenamiento basado en
el TCCC para preparar a 1317 médicos de combate para el despliegue en
Iraq y Afganistán. De los 140 médicos que se desplegaron posteriormente
en Iraq por un periodo de un año, “el 99% indicó que los principios
aprendidos en el curso TCCC le ayudó con el manejo de heridos durante
su despliegue.”23 (Sohn 2006)
El diario escrito por Holcomb
et al sobre heridos en combate en Iraq y Afganistán documentó que las
fuerzas estadounidenses en estos conflictos están experimentando la
mayor tasa de supervivencia de su historia. Ellos identificaron el TCCC
como uno de los mayores factores responsables de alcanzar este hito.”
24
El Tratado de Eastridge sobre
el reciente desarrollo de Sistemas de Trauma en Teatros Conjuntos
afirma: “Otros cursos como el Tactical Combat Casualty Care, Cirugía de
Emergencia de Guerra, y el Curso de Manejo del Trauma en Combate de
las Fuerzas Conjuntas, han revolucionado la forma de entrenamiento de
los proveedores médicos para el despliegue en tiempo de guerra.” 25
Beekley y sus colegas publicaron recientemente un documento
repasando las mayores lecciones quirúrgicas aprendidas en los
conflictos actuales. Nueve de los 19 avances que se discutieron fueron
estrategias de manejo en combate implementadas por la mayor parte por
las directrices del TCCC.” 26
Quizás la intervención
individual más exitosa del TCCC ha sido la reintroducción generalizada
del uso del torniquete en combate. Pese a que no se está yendo a la
GWOT con torniquetes modernos, las tropas del Ejército estadounidense
actualmente transportan de forma rutinaria torniquetes bien hechos en
combate. Se ha comprobado la efectividad extraordinaria de los
torniquetes en el salvamento de vidas de heridos con trauma aislado en
una extremidad27 con muy pocas complicaciones2728. Otras intervenciones
del TCCC como las vías aéreas nasofaríngeas, antibióticos orales,
descompresión torácica de un neumotórax a tensión, y las vías aéreas
quirúrgicas, no tiene una efectividad probada, pero también ayudan a
reducir tanto las necesidades de entrenamiento como la cantidad de
equipo médico acarreado por el personal médico de combate comparados
con las técnicas previas del manejo del trauma en combate.” 6
Un documento reciente de
Mabry y McManus publicado en Medicina de Cuidados Críticos ha
reflejado que “El nuevo concepto del Tactical Combat Casualty Care ha
revolucionado el manejo de heridos de combate en el entorno táctico
prehospitalario.” 29 (Mabry 2008)
Una carta del Dr. Jeff
Salomone (Presidente del Subcomité Prehospitalario del Comité de Trauma
del Colegio Americano de Cirujanos) al Secretario Asistente de Defensa
para Asuntos de Salud en el 10 de junio de 2008 afirma: Escribo para
dar mi enhorabuena por los recientes avances espectaculares en la
aplicación de los cuidados prehospitalarios por los militares
estadounidenses. Múltiples publicaciones recientes demuestran que el
Tactical Combat Casualty Care está salvando vidas en el campo de
batalla.” 30
En palabras de dos
médicos de combate de las Fuerzas Especiales experimentados: “El TCCC
identifica las causa de mortalidad en combate y los procedimientos
esenciales para su tratamiento (Ej., torniquetes, punción torácica,
etc.) a ayudado sobremanera al médico a centrarse en la utilización
del espacio cúbico de su equipo para los tratamientos vitales más
relevantes” 31
En Anales de Cirugía,
Holcomb et al examinando las primeras 82 bajas de Operaciones
Especiales en la Guerra Global Contra el Terror encontró que dos
tercios de los individuos de los 12 que murieron de heridas que eran
potencialmente prevenibles pudieron salvarse simplemente por la
apropiada aplicación de los principios del TCCC. 32 (Holcomb 2007).
El TCCC en el Departamento de Defensa de Estados Unidos
Un indicador del dramático éxito del TCCC en combate
ha sido la ràpida expansión del espectro de usuarios en los años
recientes. La orden del USSOCOM de entrenamiento en TCCC para sus
fuerzas en 200533 y, en colaboración con el USAISR, ESTABLEERON LA
Iniciativa de Transición a una trayectoria rápida hacia un nuevo
entrenamiento y equipamiento TCCC para sus unidades. 21
El BUMED en la revisión que dirigió del TCCC en 2006/2007 encontró que
actualmente el TCCC es utilizado no solamente por las unidades de
Operaciones Especiales, sino por el resto de las unidades
convencionales del Ejército de Estados Unidos. 34-38, 6, 7 Desde
febrero de 2009, el Ejército está ahora ordenando que todos los
miembros de los departamentos médicos realicen un entrenamiento en
trauma previo al despliegue que incluya el TCCC.
En Marzo de 2009, un memorándum del Dr. Ward Cascells, el Secretario
Asistente de Defensa par Asuntos de Salud, recomendó a los servicios
militares que el TCCC sea usado como el estándar para el entrenamiento
del personal médico de combate en el Ejército para el manejo del trauma
en el entorno táctico prehospitalario. (Cascells 2009)
| Este incremento en 2009 demuestra que los conceptos básicos del TCCC están sonando y están teniendo éxito en el campo de batalla. Pese a esto, los informes publicados de bajas con heridas potencialmente prevenibles corresponden a entre el 18-28% de todas las bajas en la GWOT,32 , dos unidades han informado de dos muertes no potencialmente prevenibles en sus unidades hasta la fecha. Ktwal informó de que a pesar de que el 75 Regimiento Ranger había sufrido 482 bajas en Iraq y Afganistán hasta el 28 de Agosto de 2008 (incluyendo 31 muertes), no habían identificado muertes no prevenibles en sus unidades Ranger- un logro verdaderamente destacable en siete años de guerra. Similarmente, Pennardt informó de ninguna muerte no potencialmente prevenible entre las 201 bajas (incluyendo 12 muertes) sufridas por su unidad desde que comenzó el presente conflicto. |
El factor común compartido por estas dos unidades
es que tienen un largo recorrido estándar de enseñanza del TCCC a cada
combatiente de sus unidades, de forma que tienen las intervenciones
salva-vidas más críticas, como los torniquetes, pueden ser realizadas
por todos y cada uno de los miembros de la unidad. Su éxito enfatiza la
necesidad de reflejar esta práctica en otras unidades de combate. La
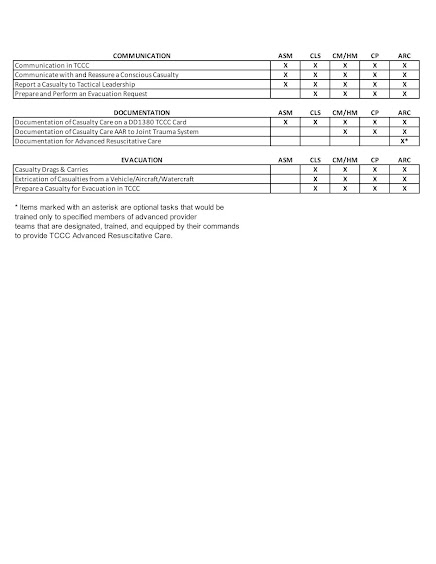
tabla 19-1 contienen el conjunto de habilidades recomendadas para el
personal médico de combate, Sanitarios (personal no-médico con
entrenamiento extra en TCCC), y todos los combatientes en el campo de
batalla.
Estas habilitaciones generales de los principios
del TCCC en el DoD son un resultado directo de los informes positivos
mencionados previamente considerando el éxito del TCCC en los campos
de batalla de la GWOT. Estos avances sostienen la gran promesa de que
el uso generalizado del TCCC en los años venideros ayudará a asegurase
de que el personal de combate médico de los Estados Unidos continuará
adquiriendo las mejores habilidades posibles para ayudar en la
asistencia de nuestros soldados heridos en el campo de batalla.
• Utilidad del TCCC en el entorno civil
Históricamente, muchas de las
lecciones aprendidas en la asistencia de heridos en el ámbito militar
han encontrado aplicación en la atención al trauma civil.
En fechas recientes, los servicios SEM civiles han
sido alertados para prestar asistencia en numerosos tiroteos en
escuelas, tiroteos en centros comerciales, y otros actos de terrorismo
que presentan factores tácticos similares a los encontrados en el
combate. La amenaza de recibir fuego hostil, teniendo que asistir a
múltiples heridos a cubierto, y tiempos prolongados de evacuación han
entrado en juego.
Las masacres de Columbine y del Tecnológico de
Virginia son ejemplos que ilustran que, incluso en entornos urbanos,
comenzar el tratamiento, y el transporte de heridos puede requerir
tácticas y entrenamiento fuera de los parámetros de los protocolos
estándar del SEM.
La adopción de las directrices aplicables del TCCC
dentro de los programas tácticos del SEM y la aplicación de estos
principios a las operaciones tácticas de los Cuerpos y Fuerzas de
Seguridad del Estado puede resultar en una mejor continuidad táctica y
vidas adicionales salvadas cuando los heridos se producen durante el
transcurso de estas operaciones.
MEDICINA PREHOSPITALARIA CIVIL vs MEDICINA TACTICA
A simple vista, ambos libros parecen lo mismo. De hecho, en su gran mayoría, son el mismo libro. La única diferencia es que el libro verde tiene unos capítulos adicionales. Pero existen unas diferencias trascendentales entre la versión regular y la versión táctica.
El ejército indentificó una lista de problemas en el contenido y la metodología de enseñanza. Cuando se mejoraron esas deficiencias, las estadísticas de sobrevivencia de pacientes severamente heridos mejoró significativamente. El resultado ha sido que hoy día tenemos las mejores estadísticas de sobrevivencia dentro de situaciones de combate en la historia reciente (desde WWII en adelante).
Muchos de los problemas que el ejército encontró son también aplicables al entorno civil y urbano. En adición, muchas de las soluciones que el ejército implementó son igualmente aplicables en las operaciones cotidianas. No me refiero a la respuesta a incidentes de tirador activo en áreas urbanas… me refiero a las operaciones rutinarias prehospitalarias e intrahospitalarias.
Sería un error ignorar estas lecciones aprendidas simplemente porque son del “ejército” y “no me aplican a mi”. Quien no conoce su historia está condenado a repetirla.
El problema
En situaciones de combate, el cuidado médico puede ocurrir bajo circunstancias extremas tales como fuego cruzado, poca iluminación, múltiples víctimas y poco equipo. En adición, en algunas ocasiones la extracción y transporte se puede retrasar si el hacerlo pone en peligro la misión y más soldados. Las guías de tratamiento que han sido diseñadas en ambientes civiles no se traducen adecuadamente a este tipo de escenario.
Aunque fuera “sentido común” desarrollar guías más específicas, el cuidado médico bajo estas circunstancias había estado basado en los mismos principios civiles:
- Proveer cuidado médico sin ninguna consideración a la situación que se desenvuelve alrededor. El mundo no se detiene porque alguien resultó herido. Las operaciones de combate continuan alrededor del herido.
- No usar torniquetes para controlar hemorragias. A pesar de que los tenían en sus equipos, los cursos iniciales enfatizaban en no usarlos, creando conflicto y retrasando su implementación.
- No usaban vendajes hemostáticos.
- Todas las víctimas de trauma significativo debían tener 2 accesos IV. En esa época se enfatizaba hacer esto en la escena aunque cada uno de los accesos vasculares tomara tiempo en lograrse.
- Tratamiento de shock hipovolémico con grandes volúmenes de cristaloides. En esa época no pensábamos que subir rápidamente la presión puede provocar la ruptura del coágulo y que grandes volúmenes diluyen los factores de coagulación.
- Ningún método de acceso IO. El acceso intravenoso no siempre es una opción.
- Manejo de la vía aérea en trauma facial mediante intubación endotraqueal. Hay pacientes que son inintubables.
- Precauciones espinales aplicadas universalmente. Prevenir las complicaciones de lo que no ha ocurrido es tan lógico como permitir que el fuego cruzado nos mate mientras le colocamos una tabla larga.
- Ninguna consideración a prevenir la hipotermia. Lo que no se mide no se puede mejorar. La hipotermia ocurre. Haga la prueba: acuéstese con ropas mojadas sobre una superficie fría y beba 1 litro de agua a temperatura ambiente (que de por sí ya están más fríos que su cuerpo). Dejo a su discreción si deja el aire acondicionado prendido o apagado. Si no siente frío, visite a su endocrinólogo favorito.
En muchos lugares esto todavía puede sonar familiar…aún hoy día.
Evolución urbana – evolución táctica
Los cambios en la medicina urbana no provienen exclusivamente de la medicina táctica. Es decir, no hemos progresado exclusivamente por lo que el mundo militar nos ha enseñado. También ha ocurrido al revés. El mundo militar ha adoptado conceptos donde el mundo civil ha sido pionero.
Lo que el mundo de trauma en combate nos está enseñando es que tenemos que desarrollar la capacidad de adaptarnos a las circunstancias del entorno y del paciente para proveer la mejor medicina posible. Nos enseña que no siempre el mismo abordaje es la solución a los problemas de un paciente determinado. Aunque suena lógico, la realidad es que el sentido común es el menos común de los sentidos.
El término táctico no significa combate
La definición de táctica es el método empleado para lograr un objetivo.
Cuando decimos táctico rápido pensamos en el color negro (o verde olivo), y en combate. Sin embargo, el término medicina táctica realmente debe evocar lo que está verdaderamente ocurriendo. Las necesidad obliga a adaptarse. Esa adaptación significa escoger los pasos necesarios para lograr los objetivos. La medicina táctica significa que nos estamos adaptando a las circunstancias para lograr los objetivos.
Lo que todo proveedor urbano debe aprender
La siguiente lista detalla algunos de los principios de la medicina de combate que muy bien podrían aplicar a cualquier paciente en un escenario urbano. No estoy diciendo que aplica a TODOS los pacientes en un entorno urbano. Hay un sinnúmero de circunstancias que pueden imitar el entorno de combate lo que nos obliga a usar tácticas similares.
- ESCENARIOS – Ningún plan sobrevive al contacto con el enemigo. Siempre es necesario adaptarse. Si el proveedor no se puede adaptar, posiblemente todos sufrirán las consecuencias.
- Torniquetes – Existen muchas razones en el entorno urbano por las cuales podemos querer detener un sangrado AHORA MISMO. La primera razón es obvia: el sangrado amenaza la vida. ¿Cuánta sangre tenemos que dejar salir antes de decidir que llegó el momento de cerrar la llave? Igualmente existen otras circunstancias tales como la necesidad de realizar otras intervenciones. A diferencia del torniquete, la presión directa requiere presión continua. Es decir, el proveedor tiene que quedarse con el paciente haciéndole presión directa. El torniquete, en cambio, se coloca y libera al proveedor para hacer otras intervenciones tales como manejar la vía aérea, respiración y circulación. En adición, permite al proveedor atender otras víctimas dentro de un incidente con múltiples víctimas que requieran atención inmediata.
- Antibióticos – Los transportes urbanos suelen ser lo suficientemente rápidos como para requerir antibióticos, pero las operaciones dentro de un desastre, o un incidente en un lugar remoto, pueden extenderse al punto donde las complicaciones asociadas a las infecciones sean la causa del compromiso del paciente.
- Resucitación con fluídos – La administración de fluídos busca lograr el mínimo de perfusión adecuada. La primera transfusión debe ocurrir luego de 1 litro de solución isotónica en pacientes con shock hemorrágico mientras se logra el control definitivo del sangrado.
- Manejo de vía aérea efectivo – El manejo de la vía aérea es una de las destrezas fundamentales del proveedor de resucitación, esté donde esté. Los pacientes con trauma maxilofacial severo con obstrucción de la vía aérea pueden necesitar una vía aérea quirúrgica. ¿Existe alguna otra opción cuando el paciente no puede proteger su propia vía aérea (incluyendo reposición) y no existe método que funcione
- Combinar buenas tácticas con buena medicina.
Otros puntos importantes que la medicina ya conoce pero que se enfatizan dentro de las operaciones de combate son:
- Diagnóstico y manejo inmediato del pneumotórax a tensión – TODOS los pacientes con pneumotórax a tensión deben ser descomprimidos inmediatamente. Esto aplica a todos los escenarios.
- Analgesia apropiada – El dolor y sufrimiento no es necesario para nada. Si el paciente es capaz de sentir dolor, el tratamiento del dolor debe comenzar de inmedidato.
Medicina Operacional
Existen muchas circunstancias donde tenemos que adaptar nuestras tácticas a diferentes circunstancias. En cada uno de los siguientes ejemplos las circunstancias imponen restricciones que, de ignorarlas, pondrían al mejor proveedor médico en aprietos si no puede adaptarse.
Medicina de combate – todo este artículo está dedicado a esto. En el ambiente urbano, los incidentes con tiradores activos y los incidentes con múltiples víctimas son aplicables.
Medicina de desastres – tiempos prolongados hasta el cuidado definitivo
Medicina en lugares remotos – operaciones de búsqueda y rescate
Conclusión
El Tactical Emergency Casualty Care, el Tactical Combat Casualty Care y el Prehospital Trauma Life Support son mutuamente complementarios. Todo profesional de la salud que provea cuidados a pacientes de trauma debe tener en su bagaje de conocimientos y experiencias las destrezas necesarias para adaptarse a las necesidades del entorno y de su paciente.
Heiskell LE, Carmona RH:
Tactical emergency medical services: an emerging subspecialty in
emergency medicine. Ann Emerg Med 1994; 23: 778-785
2 Bellamy RF: How shall we train for combat casualty care? Mil Med 1987 Dec; 152(12): 617-21
3 Baker MS: Advanced trauma life
support: is it acceptable stand-alone training for military medicine?
Mil Med 1994 Sep; 159(9): 581-90
4 Butler FK, Hagmann J, Butler EG: Tactical Combat Casualty Care in Special Operations. Mil Med 1996;161(Supp):1-16
5 Richards TR: Commander, Naval Special Warfare Command letter 1500 Ser 04/0341; 9 April 1997
6 Butler FK, Holcomb JB, Giebner
SG, McSwain NE, Bagian J: Tactical Combat Casualty Care 2007: Evolving
Concepts and Battlefield Experience. Milit Med 2007; 172(S):1-19
7 Holcomb, John B: The 2004 Fitts Lecture: Current Perspectives on Combat Casualty Care. J Trauma 2005; 59:990-1002
8 Butler FK: Tactical Medicine Training for SEAL Mission Commanders. Milit Med 2001; 166: 625-631
9 DeLorenzo, RA: Medic for the millennium: the U.S. Army 91W health care specialist. Mil Med 2001Aug; 166(8): 685-8
10 Pappas CG: The Ranger Medic. Mil Med 2001; 166: 394-400
11 Allen RC, McAtee JM:
Pararescue Medications and Procedures Manual. Air Force Special
Operations Command Publication; January 1999
12 Malish RG: The preparation of a Special Forces company for pilot recovery. Milit Med 1999; 164: 881-884
13 Krausz MM: Resuscitation
Strategies in the Israeli Army. Presentation to the Institute of
Medicine Committee on Fluid Resuscitation for Combat Casualties. 17
September 1998
14 McDevitt I: Tactical Medicine. Boulder, CO; Paladin Press; 2001
15 McSwain NE, Frame S, Paturas JL, eds: Prehospital Trauma Life Support Manual. Akron, Mosby, Fourth Edition, 1999
16 McSwain NE, Frame S, Salome
JP, eds: Prehospital Trauma Life Support Manual. Akron, Mosby, Fifth
Edition, 2003 (Second Printing)
17 McSwain NE, Salome JP, eds: Prehospital Trauma Life Support Manual. Akron, Mosby, Sixth Edition, 2006
18 Tarpey M: Tactical Combat
Casualty Care in Operation Iraqi Freedom. U.S. Army Medical Department
Journal 2005; April-June:38-41
19 Gresham J: The Year in Military and Veteran's Medicine; 2005-2006
20 Bottoms M: Tactical Combat
Casualty Care - Saving Lives on the Battlefield. Tip of the Spear
(Command Publication of the U.S. Special Operations Command); June,
2006:34-35
21 Butler FK, Holcomb JB: The
Tactical Combat Casualty Care Transition Initiative. U.S. Army Medical
Department Journal. April-June;2005
22 Brown BD: Letter of
Commendation to Army Medical Command. Commander, U.S. Special
Operations Command letter of 17 August 2005
23 Sohn VY, Miller JP, Koeller
CA, et al: From the combat medic to the forward surgical team: the
Madigan Model for improving trauma readiness of brigade combat teams
fighting the global war on terror. J Surg Res 2007;138:25-31
24 Holcomb JB, Stansbury LG,
Champion HR, Wade C, Bellamy RF: Understanding Combat Casualty Care
Statistics. J Trauma 2006;60:397-401
25 Eastridge BJ, Jenkins D,
Flaherty S, Schiller H, Holcomb JB: Trauma system development in a
theater of war: experiences from Operation Iraqi Freedom and Operation
Enduring Freedom. J Trauma 2006;1366-1373
26 Beekley AC, Starnes BW, Sebesta JA: Lessons Learned from modern Military Surgery.
Surg Clin N Am 2007;87:157-184
27 Kragh JF, Walters TJ, Baer,
DJ, et al: Survival with emergency tourniquet use to stop bleeding in
major limb trauma. Ann Surg 2009;249:1-7
28 Kragh JF, Walters TJ, Baer
DG, Fox CJ, Wade CE, Salinas J, Holcomb JB: Practical use of emergency
tourniquets to stop bleeding in major limb trauma. J Trauma
2008;64:S38-S50
29 Mabry R, McManus JG: Prehospital advances in the management of severe penetrating trauma. Crit Care Med 2008;36:S258-266
30 Salomone J: Letter to Assistant Secretary of Defense for Health Affairs dtd 10 June 2008
31 Hetzler MR, Ball JA: Thoughts on aid bags: Part One. Journal of Special Operations Medicine 2008;47-53
32 Holcomb JB, McMullen NR,
Pearse L, Caruso J, Wade CE, Oetjen-Gerdes L, Champion HR, Lawnick M,
Farr W, Rodriguez S, Butler FK: Causes of Death in Special Operations
Forces in the Global War on Terror. Annals of Surgery 2007;245:986-991
33 Brown BD: Special Operations
Combat Medic Critical Task List. Commander, U.S. Special Operations
Command letter of 9 March 2005
34 Bureau of Medicine and Surgery (Navy Surgeon General): Tactical Combat Casualty Care Training; message of 111622Z Dec 2006
35 U.S. Marine Corps Message
02004Z Aug 06: Tactical Combat Casualty Care (TCCC) and Combat
Lifesaver (CLS) Fundamentals, Philosophies, and Guidance
36 U.S. Coast Guard message 221752Z Nov 2006: Tactical Medical Response Program
37 Hostage GM: USSOCOM visit to
the Pararescue medical course at Kirtland AFB Sept 05; Air Force
Education and Training Command letter 8 Sept 05.
38 Kiley KC : Operational Needs
Statement for Medical Simulation Training Centers for Combat Lifesavers
and Tactical Combat Casualty Care Training. Army Surgeon General
Letter DASG-ZA of 1 Sept 2005
39 All Army Activities Message
0902031521Z: Mandatory Pre Deployment Trauma Training for Army Medical
Department Personnel; 3 February 2009
40 Kelly JF, Ritenhour AE,
McLaughlin DF, et al: Injury severity and causes of death from
Operation Iraqi Freedom and Operation Enduring Freedom: 2003-2004
versus 2006. J Trauma 2008;64:S21-S27
41 Kotwal R, Montgomery H: TCCC
in the 75th Ranger Regiment. Presentation at the TCCC First Responder
Conference; September 2008
42 Pennardt A: TCCC in One Special Operations Unit; Presentation at CoTCCC Meeting; 3 February 2009
43 Casscells W: Tactical Combat Casualty Care. Assistant Secretary of Defense for Health Affairs memo; 4 March 2009
Instructor Materials
TCCC Courses and Instructor Certification through the National Association of Emergency Medical Technicians (NAEMT)
TCCC FOR MEDICAL PROVIDERS
TCCC FOR ALL SERVICEMEMBERS
TCCC vs CLS: which protocol is worth choosing in military training
Text: Hlib BITYUKOV
Photo: Matteї BATRUCH
Recently, there has been much debate over which system to use to train military to provide first aid. People more experienced in international standards choose systems used in NATO member states. Then the question arises which one is best for our military: ТССС or CLS.
The first acronym ТССС (Tactical Combat Causality Care) is a standardized, systematic approach aimed at treating potentially preventable causes of death on the battlefield. This is a guideline of actions arranged in the correct sequence.
Unlike civilian medicine it is not just a certain algorithm of actions, it also presupposes a tactical component. It provides a overall understanding of the battlefield and differentiation of different actions at various stages of a battle or its parts. ТССС protocol is available for public view onthe National Association of Emergency Medical Technicians in US (NAEMT)website.
The algorithm of actions for trauma care provided on the battlefield was adopted in the late 1990s in the USA. After the United States’ invasion of Afghanistan in 2001, there were many lifesaving advances in battlefield trauma care and this protocol was expanded and adopted as a basis for all medical personnel in US and later in NATO member states.
Now the ТССС protocol is reviewed annually and recommendations based on the most recent casualty information are issued in spring. You can see the latest changes and recommendations for battlefield trauma care on the NAEMT site.
All the internationally applicable guidelines and protocols of pre-hospital casualty care to some extent are based on a specific algorithm of actions, the emphasis of which is to support vital functions such as breathing and blood circulation. This is A-B-C protocol – Airways, Breathing, Circulation.The battlefield introduces certain changes to this protocol. Primarily, it presupposes critical bleeding control, which is a major cause of premature death and disability on the battlefield, considering the fact that the casualty and everybody else are at risk of getting injured.
Tactical medicine differs from civilian medicine in terms of trauma types or wound types, surroundings, the ability to provide casualty care and the time necessary for casualty evacuation (sometimes it is much longer under combat conditions).
Tactical medicine is built around three definitive phases of casualty care which are fully compliant with ТССС protocols.
- Care under fire. It is a situation where both the casualty and the care provider are in danger from enemy fire and aims at minimizing the number of casualties. Care in this phase depends on the scarce equipment carried by each military.
- Tactical field care. Tactical field care is rendered once the casualty and the care provider are no longer under hostile fire. Medical equipment is still limited to that carried into the field by the care provider or other mission personnel. Care in this phase depends on time prior to evacuation, which may range from a few minutes to many hours.
- Tactical evacuation care. Tactical evacuation care is rendered during evacuation. Often but not always this may include qualified professionals and minimum amount of necessary equipment.
These standards are used not only for training military units. They are also mandatory for police and emergency medical technicians.
ТССС protocols unlike civilian medicine use MARCH algorithm (Massive Hemorrhage-Airways-Respiration-Circulation-Hypothermia), however the essence of this approach is pretty much the same as in С-А-В-С algorithm.
This protocol is a guideline for medical personnel and military who have passed the necessary medical training. It includes intravenous or intraosseous fluid resuscitation, use of anti-hemorrhagic or hemostatic agents such as tranexamic acid, colloidal solutions, analgesia such as ketamine or morphine, antibiotics and medical equipment, which is not available for soldiers.
It is important to realize that a combat lifesaver is not a professional medic and his first priority is to fight. First of all, he is a soldier. Primarily, the military should be trained to return fire and save lives depending on the combat conditions.
Therefore, “Combat Lifesaver course” (CLS) was developed to train people how to provide first aid. This course was adapted for all military branches and is compliant with ТССС protocols and recommendations.
First, the course implies that a combat lifesaver has no medical knowledge or skills sufficient for complex medical procedures, he is limited in the number of medical equipment available on the battlefield, and time following traumatic injury being sustained by a casualty up to their transfer to professional medical personnel may range from a few minutes to many hours.
This course is internationally recognized and was first introduced by the US Army for those who need medical care under effective enemy fire.
The course is also divided into three definite phases of providing casualty care:
Care under fire. The course takes into account that the first priority of a soldier while under fire is to continue firing at the enemy and try to prevent further casualties, to return fire and kill the enemy, to move to a safe location from enemy fire and stop life threatening bleeding.
Tactical field care.The course is based on simple actions to ensure vital functions: critical bleeding control, rapid airway management, breathing and chest examination, stabilizing blood flow; and does not include medical actions that require special skills and knowledge. It includes tactical elements as well as proving first aid. However, this care is based on the available medical equipment carried into the field by individual soldiers in his or her individual first aid kits (IFAKs).
Apart from medical skills, the course involves tactical component practice with the emphasis on military unit specifics, and focuses more on casualty care under fire.
Adapted “Combat Lifesaver course” (CLC), conducted by “Patriot Defence”, lasts for 16 hours, 2.5 of which are dedicated to care under fire.
In addition, the course was developed with the idea that each combat lifesaver could and should be able to provide first aid and be a link between the casualty and medical personnel, including military doctor assistance if a combat lifesaver has no priority military tasks.
Combat Lifesaver coursegives a possibility to save lives of casualties on prehospital stage. This course must become mandatory for all law enforcement agencies, such as the Security Service, the Armed Forces, the National Guard, the State Border Guard Service, Police Service, the Administration of State Guard of Ukraine, etc.
Comparing core skills requirements according to CLS and TCCC training course
|
CLS
|
TCCC
|
Casualty care on the battlefield is divided into definitive phases
|
V
|
V
|
Algorithm С-А-В-С (MARCH)
|
V
|
V
|
Combat Application Tourniquet
|
V
|
V
|
Nasopharyngeal airway
|
V
|
V
|
Occlusive dressings
|
V
|
V
|
Needle decompression
|
V
|
V
|
Hemostatic dressings
|
V
|
V
|
Bandaging
|
V
|
V
|
Check for additional wounds
|
V
|
V
|
Prevention of hypothermia
|
V
|
V
|
Documentation of care
|
V
|
V
|
Monitoring the casualty
|
V
|
V
|
Requesting further medical assistance.
|
V
|
V
|
Intravenous/intraosseous fluid resuscitation
| |
V
|
The use of drugs such as tranexamic acid, ketamine, morphine
| |
V
|
Colloidal solutions
| |
V
|
Burns or fractures care
| |
V
|
TCCC vs CLS: which protocol is worth choosing in military training
Text: Hlib BITYUKOV
Photo: Matteї BATRUCH
Recently, there has been much debate over which system to use to train military to provide first aid. People more experienced in international standards choose systems used in NATO member states. Then the question arises which one is best for our military: ТССС or CLS.
The first acronym ТССС (Tactical Combat Causality Care) is a standardized, systematic approach aimed at treating potentially preventable causes of death on the battlefield. This is a guideline of actions arranged in the correct sequence.
Unlike civilian medicine it is not just a certain algorithm of actions, it also presupposes a tactical component. It provides a overall understanding of the battlefield and differentiation of different actions at various stages of a battle or its parts. ТССС protocol is available for public view onthe National Association of Emergency Medical Technicians in US (NAEMT)website.
The algorithm of actions for trauma care provided on the battlefield was adopted in the late 1990s in the USA. After the United States’ invasion of Afghanistan in 2001, there were many lifesaving advances in battlefield trauma care and this protocol was expanded and adopted as a basis for all medical personnel in US and later in NATO member states.
Now the ТССС protocol is reviewed annually and recommendations based on the most recent casualty information are issued in spring. You can see the latest changes and recommendations for battlefield trauma care on the NAEMT site.
All the internationally applicable guidelines and protocols of pre-hospital casualty care to some extent are based on a specific algorithm of actions, the emphasis of which is to support vital functions such as breathing and blood circulation. This is A-B-C protocol – Airways, Breathing, Circulation.The battlefield introduces certain changes to this protocol. Primarily, it presupposes critical bleeding control, which is a major cause of premature death and disability on the battlefield, considering the fact that the casualty and everybody else are at risk of getting injured.
Tactical medicine differs from civilian medicine in terms of trauma types or wound types, surroundings, the ability to provide casualty care and the time necessary for casualty evacuation (sometimes it is much longer under combat conditions).
Tactical medicine is built around three definitive phases of casualty care which are fully compliant with ТССС protocols.
- Care under fire. It is a situation where both the casualty and the care provider are in danger from enemy fire and aims at minimizing the number of casualties. Care in this phase depends on the scarce equipment carried by each military.
- Tactical field care. Tactical field care is rendered once the casualty and the care provider are no longer under hostile fire. Medical equipment is still limited to that carried into the field by the care provider or other mission personnel. Care in this phase depends on time prior to evacuation, which may range from a few minutes to many hours.
- Tactical evacuation care. Tactical evacuation care is rendered during evacuation. Often but not always this may include qualified professionals and minimum amount of necessary equipment.
These standards are used not only for training military units. They are also mandatory for police and emergency medical technicians.
ТССС protocols unlike civilian medicine use MARCH algorithm (Massive Hemorrhage-Airways-Respiration-Circulation-Hypothermia), however the essence of this approach is pretty much the same as in С-А-В-С algorithm.
This protocol is a guideline for medical personnel and military who have passed the necessary medical training. It includes intravenous or intraosseous fluid resuscitation, use of anti-hemorrhagic or hemostatic agents such as tranexamic acid, colloidal solutions, analgesia such as ketamine or morphine, antibiotics and medical equipment, which is not available for soldiers.
It is important to realize that a combat lifesaver is not a professional medic and his first priority is to fight. First of all, he is a soldier. Primarily, the military should be trained to return fire and save lives depending on the combat conditions.
Therefore, “Combat Lifesaver course” (CLS) was developed to train people how to provide first aid. This course was adapted for all military branches and is compliant with ТССС protocols and recommendations.
First, the course implies that a combat lifesaver has no medical knowledge or skills sufficient for complex medical procedures, he is limited in the number of medical equipment available on the battlefield, and time following traumatic injury being sustained by a casualty up to their transfer to professional medical personnel may range from a few minutes to many hours.
This course is internationally recognized and was first introduced by the US Army for those who need medical care under effective enemy fire.
The course is also divided into three definite phases of providing casualty care:
Care under fire. The course takes into account that the first priority of a soldier while under fire is to continue firing at the enemy and try to prevent further casualties, to return fire and kill the enemy, to move to a safe location from enemy fire and stop life threatening bleeding.
Tactical field care.The course is based on simple actions to ensure vital functions: critical bleeding control, rapid airway management, breathing and chest examination, stabilizing blood flow; and does not include medical actions that require special skills and knowledge. It includes tactical elements as well as proving first aid. However, this care is based on the available medical equipment carried into the field by individual soldiers in his or her individual first aid kits (IFAKs).
Apart from medical skills, the course involves tactical component practice with the emphasis on military unit specifics, and focuses more on casualty care under fire.
Adapted “Combat Lifesaver course” (CLC), conducted by “Patriot Defence”, lasts for 16 hours, 2.5 of which are dedicated to care under fire.
In addition, the course was developed with the idea that each combat lifesaver could and should be able to provide first aid and be a link between the casualty and medical personnel, including military doctor assistance if a combat lifesaver has no priority military tasks.
Combat Lifesaver coursegives a possibility to save lives of casualties on prehospital stage. This course must become mandatory for all law enforcement agencies, such as the Security Service, the Armed Forces, the National Guard, the State Border Guard Service, Police Service, the Administration of State Guard of Ukraine, etc.
Comparing core skills requirements according to CLS and TCCC training course
|
CLS
|
TCCC
|
Casualty care on the battlefield is divided into definitive phases
|
V
|
V
|
Algorithm С-А-В-С (MARCH)
|
V
|
V
|
Combat Application Tourniquet
|
V
|
V
|
Nasopharyngeal airway
|
V
|
V
|
Occlusive dressings
|
V
|
V
|
Needle decompression
|
V
|
V
|
Hemostatic dressings
|
V
|
V
|
Bandaging
|
V
|
V
|
Check for additional wounds
|
V
|
V
|
Prevention of hypothermia
|
V
|
V
|
Documentation of care
|
V
|
V
|
Monitoring the casualty
|
V
|
V
|
Requesting further medical assistance.
|
V
|
V
|
Intravenous/intraosseous fluid resuscitation
| |
V
|
The use of drugs such as tranexamic acid, ketamine, morphine
| |
V
|
Colloidal solutions
| |
V
|
Burns or fractures care
| |
V
|
TCCC 170906 NAEMT TCCC Courses v3-01
"CONTUDENTE CARTA DEL DOCTOR FRANK BUTLER, EN DONDE LE DA RESPALDO A LA NAEMT Y SE ORDENA A MILITARES A DAR LA FORMACION TCCC TACTICAL COMBAT CASUALTY CARE POSTERIOR A ACREDITARSE CON LA NAEMT, SE HAN IDENTIFICADO RIESGOS REALES EN EL CAMPO DE BATALLA POR LA MALA INFORMACION (DESINFORMACION) A LA QUE HAN SIDO SOMETIDOS LOS SOLDADOS"
A Letter from Dr. Frank Butler Regarding TCCC for Medical Personnel (TCCC-MP) Courses Offered by NAEMT
The recent 16 years of war in Afghanistan and Iraq have enabled the US Military to make remarkable advances in battlefield trauma care. Since the large majority of combat fatalities occur before the casualty ever reaches a medical treatment facility, the importance of prehospital care is paramount in reducing preventable deaths. Tactical Combat Casualty Care (TCCC) has demonstrated great success in reducing preventable deaths and has become the standard for battlefield trauma care, both in the US Military and in the militaries of many allied nations.
In a moving presentation at last week's meeting of the Committee on TCCC,
US Army medic SSG Adam Hartswick described how his TCCC training saved his
life when he was wounded by an IED on a mission in Afghanistan in 2013. After this experience, in spite of the ongoing physical challenges from his wounds, he has now dedicated himself to training others in TCCC.
The attached links and their corresponding documents, including a 2013 letter from Secretary of Defense James Mattis to the Service Chiefs, written while he was the Commander ofthe US Central Command, highlights the importance of TCCC training.
All of the US Armed Services have now endorsed TCCC concepts, but due to
the divided authorities and distributed responsibilities in the DoD organizational structure, TCCC is still not being optimally trained or equipped in our combat forces. This training gap has been noted both in two recent surveys of prehospital trauma care in Afghanistan and in the Joint Trauma System's ongoing combat casualty care performance improvement process.
The need for better TCCC training was a major topic of discussion at last
week's CoTCCC meeting in San Antonio, and I am forwarding the items listed
below for your consideration:
1. Many courses that purport to train TCCC have been shown to contain
incorrect messaging. This suboptimal training this has been directly
responsible for adverse outcomes in our combat casualties. As recommended by
the Director of the Joint Trauma System in the attached 2015 White Paper,
TCCC training for medical personnel should be accomplished through the use
of standardized, high-quality, internationally recognized TCCC-MP courses,
such as those offered by the National Association of Emergency Medical
Technicians (NAEMT).
2. The attached presentation from last week's CoTCCC meeting reviews some
of the adverse casualty outcomes that have occurred as a result of incorrect
messaging in training courses that were supposed to be teaching TCCC. It
also outlines the 20-year strategic partnership between TCCC and NAEMT and
describes how NAEMT, a civilian organization, first began conducting TCCC
training in 2009. As noted in the presentation, COL Jim Geracci, the former
Army III Corps Command Surgeon, implemented the use of NAEMT TCCC-MP courses
to train his command's physicians, PAs, and medics. Another perspective on the need for high-quality, standardized TCCC training was provided by CDR Carl Goforth when he was at the Marine Corps Combat Development Command - his paper is also attached.
3. The attached NAEMT TCCC Fact Sheet provides an overview of NAEMT and
how their TCCC-MP courses are conducted.
If your military unit would like to begin training TCCC-MP courses, or if
you are currently conducting TCCC courses without NAEMT certification,
please contact Ms. Corine Curd at NAEMT (601-924-7744 or
corine.curd@naemt.org ) for information on how your unit can become a
certified NAEMT training site and begin issuing TCCC-MP cards that carry the
endorsement of the American College of Surgeons Committee on Trauma and the
NAEMT as well as the CoTCCC and the Joint Trauma System.
Discussions are also ongoing with the Uniformed Services University of the
Health Sciences and the Defense Medical Readiness Training Institute and
TCCC courses may be included in the course offerings of the Military Training Network in the near future.
V/R -
Frank K. Butler, MD
CAPT MC USN (Ret)
Chairman
Committee on Tactical Combat Casualty Care
Chief
Prehospital Trauma Care
Joint Trauma System
Adjunct Professor of Military and Emergency Medicine Uniformed Services
University of the Health Sciences
@SUBITUSINT #SUBITUSINT
https://emssolutionsint.blogspot.com/2019/06/subitus-international.html
https://www.facebook.com/SUBITUSINT/
+1 849-849-8576 +34 671454059
subitusint@gmail.com
Nuestros Productos y Servicios
Formacion
Somos Centro de Entrenamiento NAEMT
Programa PreHospital Trauma Life Support PHTLS
Programa Advanced Medical Life Support AMLS
Programa Tactical Combat Casualty Care TCCC
Programa Tactical Emergency Casualty Care TECC
Somos Centro de Entrenamiento American Heart Association AHA
Basic Life Suppor BLS
Advanced Cardiac Life Support ACLS
Advanced Cardiac Life Support for Experience Provider ACLS EP
Pediatric Advanced Cardiac Life Support PALS
Somos Centro de Entrenamiento ESCI
Somos Centro de Entrenamiento ASHI and Medic First Aid
Estamos adosados a los programas BCon Bleeding Control Basic del Colegio Americano de Cirujanos
Estamos adosados a los programas BCon de First Care Provider del Department Homeland Security de los Estados Unidos
Estamos Autorizados a utilizar el logo y guias del Comite Tactical Emergency Casualty Care
Nuestros Clientes
Helidosa Aviation Group AEROAMBULANCIA
Hospiten Santo Domingo y Hospiten Bavaro
Clinica Corazones Unidos
Embajada de Canada
TRASTORNO ESPECTRO AUTISMO y URGENCIAS PDF