Los autores realizaron un ensayo aleatorizado por grupos cruzado entre seis servicios de paramédicos canadienses para evaluar la desfibrilación DESD y CV en comparación con la desfibrilación estándar en pacientes adultos con fibrilación ventricular refractaria durante un paro cardiaco extrahospitalario. Los pacientes fueron tratados con una de estas tres técnicas según la estrategia asignada aleatoriamente a cada servicio de paramédicos. El objetivo primario fue la supervivencia hasta el alta hospitalaria. Los objetivos secundarios incluyeron la terminación de la fibrilación ventricular, el retorno a la circulación espontánea y un buen resultado neurológico, definido como una puntuación en la escala de Rankin modificada de 2 o menos al alta hospitalaria.
Se incluyeron un total de 405 pacientes antes de que la junta de monitorización de datos y seguridad detuviera el ensayo debido a la pandemia por SARS-CoV-2. Un total de 136 pacientes (33,6%) fueron asignados a recibir desfibrilación estándar, 144 (35,6%) a recibir desfibrilación CV y 125 (30,9%) para recibir DESD. La supervivencia al alta hospitalaria fue más frecuente en el grupo DESD que en el grupo estándar (30,4% frente al 13,3%; riesgo relativo, 2,21; intervalo de confianza [IC] del 95%: 1,33-3,67) y más común en el grupo CV que en el grupo estándar (21,7% frente al 13,3%; riesgo relativo 1,71; IC 95%: 1,01-2,88). La desfibrilación DESD, pero no la CV, se asoció con un mayor porcentaje de pacientes con un buen resultado neurológico que la desfibrilación estándar (riesgo relativo 2,21 [IC 95%: 1,26-3,88] y 1,48 [IC 95%: 0,81-2,71], respectivamente).
Los autores concluyen que, entre los pacientes con fibrilación ventricular refractaria, la supervivencia al alta hospitalaria fue más frecuente entre los que recibieron desfibrilación DESD o CV que entre los que recibieron desfibrilación estándar.
Comentario
Sin dudas uno de los grandes trabajos presentados en el congreso de la AHA de 2022. Casi la mitad de los pacientes que son atendidos por una parada cardiorrespiratoria (PCR) extrahospitalaria presentan una fibrilación ventricular (FV) refractaria, definida por la ausencia de retorno hasta la circulación espontánea tras 3 desfibrilaciones, lo cual se asocia a un pésimo pronóstico. Aunque el tratamiento antiarrítmico se utiliza en estos casos, ni la lidocaína ni la amiodarona han conseguido mejorar la supervivencia de estos pacientes. En los últimos años, se ha extendido el uso de dispositivos de oxigenación con membrana extracorpórea (ECMO) para facilitar la reanimación cardiopulmonar (ERCP), consiguiendo un incremento de la supervivencia significativa. Sin embargo, este tipo de terapia no está exenta de una gran complejidad que se acompaña de complicaciones, alto gasto sanitario y obliga a una importante organización asistencial. Cuando todo hacía pensar que la única vía para mejorar la supervivencia de estos pacientes estaría ligada a la extensión de los programas ERCP, este grupo de investigadores canadienses han diseñado este trabajo, en el cual son capaces de demostrar un incremento mayor de la supervivencia que los alcanzados en los estudios con ERCP, con un protocolo simple, práctico y barato.
"Tras la publicación de los resultados del estudio DOSE VF, urge modificar los protocolos de atención a la parada cardiorrespiratoria", señala @Auribarri. #BlogSEC @jovenesSEC
Tuitéalo
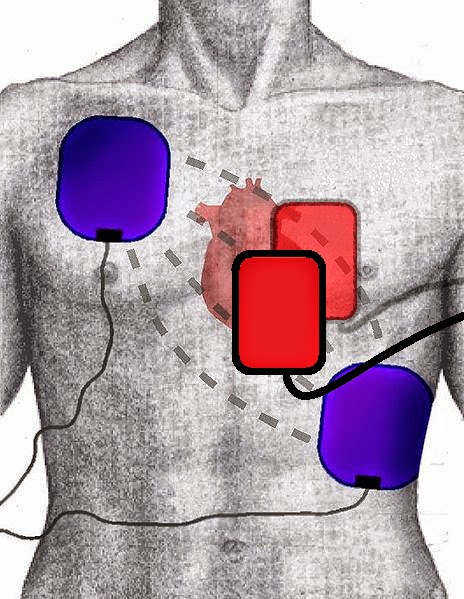
Desde el punto de vista fisiopatológico, el cambio de configuración tiene todo el sentido el mundo. Estudios previos han mostrado que cuando la desfibrilación no logra terminar la FV, esta se reanuda en la región de menor voltaje donde ha recibido el menor gradiente de corriente. La ubicación anatómica del ventrículo izquierdo, una estructura posterior, es la región del corazón que está más lejos de la línea creada entre los electrodos en la configuración anterolateral. La desfibrilación anteroposterior puede resultar en un gradiente de voltaje más alto en la parte posterior del ventrículo izquierdo, donde es más probable que la FV no se termine o se reinicie tras la desfibrilación con configuración anterolateral. Por otra parte, puede que con la DESD influya también el aumento de energía generada por la segunda descarga. Además, el rápido cambio del frente de onda que se genera durante la DESD puede hacer más vulnerable al miocardio.
Estos cambios en la dirección del frente de descarga no son nuevos y se llevan utilizando desde hace años. El estudio EPIC ya demostró que la desfibrilación con configuración anteroposterior era superior a la estándar en pacientes con fibrilación auricular y, en su discusión, los autores también defendían que, de esta manera, se permite aumentar el miocardio atravesado por la corriente de choque. Otro ejemplo práctico es la configuración utilizada en las terapias de desfibrilación de los DAI. Habitualmente, en la mayoría de los protocolos, en la cuarta o quinta terapia se suele invertir la polaridad de la descarga, ya que esto ha demostrado terminar la FV con mayor probabilidad.
"Las descargas secuenciales rápidas con dos desfibriladores, utilizando una configuración anterolateral y otra anteroposterior, mejoran el pronóstico de los pacientes con una FV refractaria", indica @Auribarri. #BlogSEC @jovenesSEC
Tuitéalo
Uno puede intentar buscar críticas a este trabajo: que si no se alcanzó el tamaño muestral por culpa de la pandemia COVID; que si no existe información sobre los cuidados posparada a nivel hospitalario; que si hasta un 10% de los paciente recibió otro tipo de desfibrilación al que se le había asignado con la aleatorización… Sinceramente en este caso, el “que si no” me parece intentar buscar tres pies al gato, y tras la publicación de estos resultados, me parece obligado empezar a implementar protocolos de cambio de configuración de desfibrilación en los pacientes con FV refractaria. Cuesta poco y se puede ganar mucho.
Referencia
Defibrillation strategies for refractory ventricular fibrillation
Sheldon Cheskes, P. Richard Verbeek, Ian R. Drennan, Shelley L. McLeod, Linda Turner, Ruxandra Pinto, Michael Feldman, Matthew Davis, Christian Vaillancourt, Laurie J. Morrison, Paul Dorian, and Damon C. Scales.
N Engl J Med. 2022 Nov 6. doi: 10.1056/NEJMoa2207304. Online ahead of print.
ADVERTENCIA
CARDIOLOGÍA HOY es el blog de la Sociedad Española de Cardiología (SEC), un foro abierto sobre actualidad médico-científica. Los contenidos publicados en este blog están redactados y dirigidos exclusivamente a profesionales de la salud. Las opiniones vertidas en este blog corresponden a los autores de los artículos y no necesariamente reflejan la opinión de la SEC. El Grupo Jóvenes Cardiólogos de la SEC no aceptará artículos y comentarios al margen de este contexto formativo y de actualización de las evidencias clínicas. Más información sobre las Normas de comportamiento del blog.
- It's a vector issue, where using four pads instead of two creates a broader energy vector.
- It's a duration issue, related to what is basically a single prolonged shock delivered by consecutive defibrillations. In that case, consecutive may be better than simultaneous.
- It's an energy issue, relating to the sheer number of joules delivered. In that case, simultaneous may be better than consecutive.
Double Sequential External Defibrillation in Out-of-Hospital Refractory Ventricular Fibrillation: A Report of Ten Cases.
Abstract
KEYWORDS:
http://www.ncbi.nlm.nih.gov/pubmed/25243771
 |
High Energy Defibrillation for Incessant Ventricular Fibrillation |
High Energy Defibrillation for Incessant Ventricular Fibrillation
http://resusreview.com/2013/high-energy-defibrillation-for-incessant-ventricular-fibrillation/Por Sheldon Cheskes, MD, CCFP (EM), FCFP
La doble desfibrilación externa secuencial (DSED) para la fibrilación ventricular (FV) refractaria ha generado un gran interés, excitación y confusión como opción de tratamiento para los pacientes que presentan una FV refractaria.
DETRÁS DE TODO ESTO
La DSED se ha estudiado durante décadas en el laboratorio de electrofisiología para pacientes con fibrilación auricular refractaria y FV refractaria. 1-8
¿Por qué los intentos de desfibrilación en curso en la FV refractaria no logran terminar la FV?
Se cree que la razón es al menos doble. A medida que persiste la FV, la energía necesaria para desfibrilar aumenta en función del tiempo, debido a los cambios inducidos por la isquemia en la velocidad de conducción y la refractariedad.
En segundo lugar, si las descargas iniciales no logran terminar la FV, la energía suministrada al corazón en fibrilación puede ser insuficiente para terminar la FV. Finalmente, a medida que avanza la reanimación, la hipoxia, la acidosis y los aumentos repentinos de catecolaminas exógenas y endógenas aumentan el consumo de oxígeno del miocardio, lo que dificulta la desfibrilación satisfactoria del ventrículo. 1-4
Las descargas desfibriladoras despolarizan efectivamente la mayor parte del miocardio fibrilado y permiten que comience la contracción muscular coordinada del corazón.
Cuando una descarga no logra terminar con la FV, la fibrilación se reanuda o reinicia invariablemente comenzando en la región de voltaje y gradiente de corriente más bajos en el miocardio.
Dada la posición habitual de las almohadillas o Parches de desfibrilación (anterior-anterior), esta región será la región posterolateral del ventrículo izquierdo, donde el vector de choque da como resultado el gradiente de voltaje más bajo.
Teniendo en cuenta la ubicación anatómica del ventrículo izquierdo, una estructura posterior, esta región es la más alejada de la línea directa entre las almohadillas de los electrodos. Como consecuencia, existen múltiples razones por las que los métodos alternativos de desfibrilación pueden tener más éxito.
Los informes de casos publicados recientemente y las series de casos múltiples han descrito resultados contradictorios para los pacientes tratados con DSED por FV refractaria. 9-15
En un análisis retrospectivo de 50 casos de DSED durante un período de tiempo de tres años, Ross et al., No informaron mejoría en el resultado primario de supervivencia neurológicamente intacta con DSED, pero no incluyeron datos sobre el momento del choque DSED o calidad CPR. 10
Beck et al. Observaron hallazgos similares, pero no informaron sobre la cuestión crítica del momento de la DSED en la FV refractaria y tampoco incluyeron datos sobre la calidad de la RCP proporcionada. 11
Los autores señalan que "DSD puede ser más eficaz si se usa antes y mediante un protocolo permanente".
Cabanas et al., Pudieron demostrar una mejor terminación de la FV empleando un protocolo prehospitalario utilizando DSED, pero no informaron ninguna mejora en la supervivencia hospitalaria, probablemente debido a la aplicación tardía de la intervención. 9
Por el contrario, Lybeck et al., Y Johnson et al., Ambos describieron informes de casos de uso temprano de DSED con resultados exitosos de supervivencia neurológicamente intacta hasta el alta hospitalaria. 12,13
La mayoría de los usos de DSED se han empleado como un esfuerzo final ad-hoc para convertir la FV refractaria, a diferencia de una aplicación temprana planificada durante la reanimación.
NUESTRA INVESTIGACIÓN
El objetivo de nuestro estudio fue explorar la relación entre el tipo de desfibrilación (estándar vs DSED), el número de intentos de desfibrilación proporcionados y los resultados de la terminación de la FV y la terminación de la FV con retorno de la circulación espontánea (ROSC) para pacientes cardíacos extrahospitalarios. Pacientes con paro cardíaco (OHCA) que se presentan en FV refractaria.
Realizamos una revisión retrospectiva de los datos recopilados prospectivamente en adultos tratados con OHCA (≥ 18 años) que se presentaron en FV y recibieron un mínimo de tres desfibrilaciones estándar sucesivas durante un período de tres años a partir del 1 de enero de 2015 en cuatro agencias de servicios de emergencias médicas en Ontario. Canadá.
Las agencias (Servicio Paramédico Regional Peel, Servicio Paramédico de la Región Halton, Servicio Paramédico Simcoe y Servicio Paramédico Toronto) brindan atención de Emergencia y transporte a una población de 4.8 millones de personas en entornos urbanos y rurales dentro de un área geográfica de 7.680 km 2.
Para evaluar la relación entre el número de intentos de desfibrilación, el modo de desfibrilación (estándar frente a DSED) y nuestras medidas de resultado de terminación de FV y terminación de FV a ROSC, realizamos un análisis de secuencia de descargas.
Primero dividimos nuestra cohorte general en dos grupos, los que solo recibieron desfibrilación estándar durante su reanimación y los que recibieron al menos un DSED como parte de su reanimación.
Para evaluar el impacto del modo de desfibrilación sobre una base de descarga por descarga, analizamos qué tipo de desfibrilación (estándar o DSED) se proporcionó a cada paciente en cada intento de desfibrilación.
Esto nos permitió tener en cuenta el tiempo variable en el que se proporcionó la DSED inicial durante cada reanimación individual.
NUESTROS RESULTADOS
Durante el período de estudio, 252 pacientes cumplieron los criterios de inclusión. De los 252 pacientes incluidos en el análisis, 201 (79,8%) recibieron desfibrilación estándar y 51 (20,2%) pacientes recibieron DSED.
La edad, el sexo, el lugar del arresto, el arresto presenciado por los servicios de emergencias médicas, el estado del testigo y la tasa de RCP por parte del espectador fueron similares entre los grupos estándar y DSED.
En general, la terminación de la FV fue similar entre la cohorte estándar y la DSED (78,1% frente a 76,5%; RR: 1,0; IC del 95%: 0,8 a 1,2).
En nuestro análisis de secuencia de descargas, cuando se consideraron los intentos tempranos de desfibrilación (intento de desfibrilación 4-8), la terminación de la FV fue mayor para los que recibieron DSED en comparación con la desfibrilación estándar (29,4% frente a 17,5%; RR: 1,7; IC del 95%: 1,1 a 2.6).
Cuando se consideraron los intentos tardíos de desfibrilación (intento de desfibrilación 9-17), la terminación de la FV fue mayor para los que recibieron DSED en comparación con la desfibrilación estándar (31,2% frente a 17,1%; RR: 1,8; IC del 95%: 1,1 a 3,0). En general, ROSC fue similar entre los grupos estándar y DSED (21,4% frente a 17,6%; RR: 0,8; IC del 95%: 0,4 a 1,6).
Cuando se consideraron los primeros intentos de desfibrilación (intento de desfibrilación 4-8), el ROSC fue mayor para los que recibieron DSED en comparación con la desfibrilación estándar (15,7% vs. 5,4%; RR: 2,9; IC del 95%: 1,4 a 5,9).
Cuando se consideraron los intentos tardíos de desfibrilación (intento de desfibrilación 9-17), las tasas de ROSC fueron similares para los que recibieron DSED en comparación con la desfibrilación estándar (1,3% frente a 0,8%; RR: 1,6; IC del 95%: 0,1 a 25,2).
Para los casos en los que DSED terminó la FV en ROSC, la mediana (rango intercuartílico) del número de desfibrilaciones estándar antes de DSED fue 4 (4, 6), en comparación con 7 (6, 9) desfibrilaciones cuando DSED no dio como resultado ROSC.
Cuando DSED terminó VF en ROSC, lo hizo con un solo DSED en el 66,7% de los casos. Estos resultados sugieren que la reanimación exitosa con DSED puede ser sensible al tiempo, con mayor éxito al comienzo de la reanimación.
Las tasas de ROSC fueron similares para los que recibieron DSED en comparación con la desfibrilación estándar (1,3% frente a 0,8%; RR: 1,6; IC del 95%: 0,1 a 25,2).
Para los casos en los que DSED terminó la FV en ROSC, la mediana (rango intercuartílico) del número de desfibrilaciones estándar antes de DSED fue 4 (4, 6), en comparación con 7 (6, 9) desfibrilaciones cuando DSED no dio como resultado ROSC.
Cuando DSED terminó VF en ROSC, lo hizo con un solo DSED en el 66,7% de los casos. Estos resultados sugieren que la reanimación exitosa con DSED puede ser sensible al tiempo, con mayor éxito al comienzo de la reanimación.
Las tasas de ROSC fueron similares para los que recibieron DSED en comparación con la desfibrilación estándar (1,3% frente a 0,8%; RR: 1,6; IC del 95%: 0,1 a 25,2).
Para los casos en los que DSED terminó la FV en ROSC, la mediana (rango intercuartílico) del número de desfibrilaciones estándar antes de DSED fue 4 (4, 6), en comparación con 7 (6, 9) desfibrilaciones cuando DSED no dio como resultado ROSC.
Cuando DSED terminó VF en ROSC, lo hizo con un solo DSED en el 66,7% de los casos. Estos resultados sugieren que la reanimación exitosa con DSED puede ser sensible al tiempo, con mayor éxito al comienzo de la reanimación.
Cuando DSED terminó VF en ROSC, lo hizo con un solo DSED en el 66,7% de los casos. Estos resultados sugieren que la reanimación exitosa con DSED puede ser sensible al tiempo, con mayor éxito al comienzo de la reanimación.
Cuando DSED terminó VF en ROSC, lo hizo con un solo DSED en el 66,7% de los casos. Estos resultados sugieren que la reanimación exitosa con DSED puede ser sensible al tiempo, con mayor éxito al comienzo de la reanimación.
LAS CONTROVERSIAS
MOMENTO DE LA INTERVENCIÓN
Una limitación de la investigación previa es la omisión de datos sobre el tiempo de DSED para pacientes con FV refractaria. En la gran mayoría de los casos descritos, la DSED se aplica tarde, ya que a menudo se usa solo después de intentos fallidos de desfibrilación estándar.
Con los esfuerzos de reanimación en curso, las condiciones para una desfibrilación exitosa se deterioran, a medida que se produce hipoxia, acidosis y una mayor administración de epinefrina.
Nuestros colegas del Consorcio de Resucitación de Minnesota también han sugerido que el momento de una intervención en la FV refractaria es fundamental para el éxito.
En un enfoque innovador para la FV refractaria, los pacientes que presentan una FV refractaria y han fallado tres intentos de desfibrilación son transferidos desde el campo con RCP mecánica directamente al laboratorio de cateterismo cardíaco.16
Si bien se obtienen resultados sobresalientes en este subconjunto de pacientes, es fundamental comprender que estos resultados no solo se basan en una excelente atención prehospitalaria y PCI / ECMO, sino también en una atención hospitalaria continua y ejemplar, ya que el 100% de estos pacientes sufren fallas multisistémicas.
Por lo tanto, la generalización del enfoque de Minnesota para la FV refractaria puede ser un desafío para la gran mayoría de las agencias del SEM. Lo que se ha demostrado que es crítico es el factor tiempo.
Para que ECMO tenga éxito, debe hacerse temprano. En el consorcio de Minnesota, la supervivencia neurológicamente intacta hasta el alta hospitalaria es casi del 100% si la ECMO se inicia dentro de los 30 minutos posteriores al paro cardíaco.
Desafortunadamente, el éxito se reduce en un 25% por cada diez minutos de retraso sobre los 30 minutos originales y es esencialmente del 0% en una hora. 17
Además, si se aplicó ECMO después de múltiples intentos fallidos de desfibrilación en el campo, la probabilidad de éxito sería mucho menor de lo que se informa actualmente.
FV REFRACTARIA O RECURRENTE: ¿IMPORTA?
La investigación en el área de la FV refractaria se ha complicado por la falta de una definición concreta de esta condición.
Existen controversias similares en la definición de terminación de FV. Lo que más importa es cómo esta diferencia afecta a los Paramédicos en el cuidado de sus pacientes de manera pragmática.
Se suele citar que la desfibrilación bifásica terminará la FV en más del 90% de los intentos de desfibrilación. 18 Lo que no está claro es cómo describimos la desfibrilación "exitosa".
La mayoría estaría de acuerdo en que la desfibrilación de FV en asistolia o PEA no se consideraría "exitosa", pero hasta el 60% de los intentos de desfibrilación dan como resultado estos ritmos sin perfusión.
De manera similar, la terminación de la FV se ha definido como la terminación de la FV dentro de los cinco segundos posteriores a la desfibrilación. 19
Esta definición histórica se remonta a 2005, antes de múltiples cambios en la provisión de CPR.
El enfoque reciente en la reanimación cardiopulmonar de alta calidad ha dado lugar a pausas extremadamente breves tras la descarga.
El artefacto de RCP hace que el uso de esta definición histórica sea problemático incluso cuando se revisan estos casos en retrospectiva. Para los paramédicos que brindan atención, lo único que importa es el ritmo en el que se encuentra el paciente después de la desfibrilación y dos minutos de RCP.
El ritmo que se produjo de forma transitoria después de la administración de la descarga no influye en el tratamiento actual de la FV refractaria. Como tal, las descripciones históricas de FV refractaria pueden incluir una colección heterogénea de casos que incluyen FV refractaria y recurrente.
DATOS AGRUPADOS DE ESTUDIOS HETEROGÉNEOS: TENGA CUIDADO CON LA INTERPRETACIÓN DE LOS RESULTADOS
El metaanálisis es el procedimiento estadístico para combinar datos de múltiples estudios. Un beneficio clave de este enfoque es la agregación de información que conduce a un mayor poder estadístico y una estimación puntual más robusta de lo que es posible a partir de la medida derivada de cualquier estudio individual.
Sin embargo, al realizar un metaanálisis, un investigador debe tomar decisiones que puedan afectar los resultados, incluida la decisión de cómo buscar estudios, la selección de estudios en función de un conjunto de criterios objetivos, el tratamiento de datos incompletos, el análisis de los datos y la contabilización de o elegir no tener en cuenta el sesgo de publicación.
Desafortunadamente, la gran mayoría de los estudios en atención prehospitalaria, y ciertamente los de DSED y FV refractaria, no son ensayos controlados aleatorios, sino series de casos, informes de casos y estudios de cohortes observacionales.20 Incluso un buen metaanálisis no puede corregir un diseño deficiente o sesgo en los estudios originales. P
or lo tanto, al interpretar los resultados de un metaanálisis de DSED en FV refractaria, observe de cerca los diseños originales del estudio y tenga cuidado al interpretar los resultados agrupados.
INVESTIGACIÓN FRENTE A APLICACIÓN EN EL MUNDO REAL: ¿CUÁL ES EL INTERVALO DE TIEMPO ÓPTIMO ENTRE DESCARGAS DSED?
Los estudios en animales sugieren que la DSED puede tener éxito al reducir el umbral de desfibrilación. 3 Investigaciones anteriores sugieren que la sincronización óptima de las dos descargas puede ser tan breve como 10 milisegundos (ms), o entre 75-125 ms, con un período de umbral de desfibrilación aumentado que existe entre 50 y 75 ms.
No se estudiaron periodos superiores a 125 ms. El período refractario conocido del músculo ventricular está entre 50-75 ms, que puede ser un período particularmente vulnerable para reintroducir la fibrilación ventricular. 21
Contrastando estos hallazgos con los de estudios anteriores en animales, Hoch et al., Han demostrado el uso exitoso de DSED en FV refractaria con descargas separadas por 0.5 a 4.5 segundos sin terapia farmacológica entre descargas exitosas y fallidas (DSED). 1
Para aquellos que realizan DSED en el campo prehospitalario, el tiempo de las descargas es generalmente heterogéneo ya que la aplicación de la intervención a menudo varía entre simultánea (presionando directamente el botón de descarga en dos desfibriladores al mismo tiempo) y secuencial (presionando el botón de descarga de dos desfibriladores de forma secuencial).
Como tal, a menudo es difícil determinar pragmáticamente la relación entre el momento exacto de los choques DSED y los resultados de interés. Nuestro grupo de investigación ha desarrollado una técnica para calcular retrospectivamente el momento de las descargas DSED durante una reanimación.
La investigación futura explorará si la optimización del marco de tiempo entre los intentos de DSED puede mejorar los resultados de la terminación de la FV y ROSC. Si el momento de las descargas de DSED en la vida real está relacionado con la eficacia de DSED,
DAÑO DEL DESFIBRILADOR: MITO O REALIDAD
Una de las preocupaciones más comunes de quienes desean iniciar DSED es la posibilidad de dañar el desfibrilador. Aunque es poco común, es posible que se produzcan daños en el desfibrilador cuando se utiliza una desfibrilación simultánea (en milisegundos). 22
El mecanismo de este daño es poco conocido. De hecho, muchas agencias del SEM no han estado preparadas para intentar DSED, ya que algunos fabricantes de desfibriladores no cubrirán la garantía del desfibrilador si se daña durante DSED. 23
Lo que sí encontré notable es la cantidad de agencias del SEM que se acercaron a mí después de nuestra presentación en NAESP que están realizando DSED con desfibrilación simultánea a pesar de la advertencia del fabricante del desfibrilador.
En realidad, la probabilidad de que esto ocurra es remota, ya que la capacidad de los seres humanos para proporcionar descargas dentro de este marco de tiempo exacto es cercana a cero. Hasta donde sabemos, nunca ha habido un caso de daño del desfibrilador cuando se ha producido una descarga secuencial, y la desfibrilación secuencial rápida no se ha asociado con daño / mal funcionamiento del desfibrilador.
DESFIBRILACIÓN EXTERNA SECUENCIAL DOBLE: ¿ES LA ENERGÍA O EL VECTOR?
En teoría, la aplicación de DSED conduce a la provisión de más energía para superar el umbral de desfibrilación creciente observado cuando los intentos de desfibrilación estándar continúan fallando. Sin embargo, es posible que el problema no sea un problema de energía.
La eficacia de DSED puede ser simplemente el plano o vector alternativo de desfibrilación proporcionado por la colocación de la almohadilla anteroposterior agregada a la colocación de la almohadilla antero-anterior estándar.
El vector o la vía del flujo de energía de desfibrilación puede ser un factor en el éxito del cambio de vector, ya que las descargas que incorporan una vía que incluye el tabique interventricular pueden requerir niveles de energía más bajos para desfibrilar, y diferentes vías pueden resultar en una mayor densidad de corriente (gradientes de voltaje) en las áreas de voltaje más bajo después de las descargas estándar. 24
Se requiere investigación adicional para determinar si el beneficio potencial de DSED está relacionado con la energía, el vector o ambos.
Un nuevo ensayo para ayudar a abordar algunos de estos problemas: Desfibrilación externa secuencial doble en FV refractaria: el ensayo controlado aleatorio DOSE VF
El estudio piloto DOSE VF es un estudio cruzado, aleatorizado por conglomerados diseñado para determinar la viabilidad de realizar un ensayo aleatorizado a gran escala en esta población de pacientes.
Específicamente, los pacientes que presentan FV y fallan en tres intentos sucesivos de desfibrilación son asignados al azar para recibir una de tres terapias: (1) reanimación continúa usando desfibrilación estándar; (2) reanimación con DSED; o (3) reanimación con cambio de vector (cambio de los electrodos de desfibrilación de la posición anterior-anterior a una anteroposterior) desfibrilación.
El resultado primario será la supervivencia hasta el alta hospitalaria. Hasta la fecha, hemos capacitado a más de 2.300 Paramédicos en Ontario en la técnica de DSED y desfibrilación por cambio de vector.
Los videos de capacitación para el estudio DOSE VF RCT utilizado por los Servicios Paramédicos Regionales de Peel se adjuntan a continuación. Todos los Paramédicos recibieron capacitación en persona utilizando una combinación de escenarios didácticos, de video y simulados antes del lanzamiento del estudio.
Todos los pacientes elegibles con FV refractaria (n = 128 hasta la fecha) en cuatro agencias de EMS participantes se han inscrito, y los paramédicos han aplicado con éxito tanto el cambio de vector como la DSED sin problemas reportados. Hemos demostrado que nuestro protocolo es factible y bien aceptado por los paramédicos en el campo.
Esperamos que el estudio piloto DOSE VF y la expansión de este ensayo a más sitios proporcionen pruebas de alto nivel en cuanto al beneficio potencial de las estrategias de desfibrilación alternativas para los pacientes que presentan una FV refractaria.
Todos los pacientes elegibles con FV refractaria (n = 128 hasta la fecha) en cuatro agencias del SEM participantes se han inscrito, y los paramédicos han aplicado con éxito tanto el cambio de vector como la DSED sin problemas reportados. Hemos demostrado que nuestro protocolo es factible y bien aceptado por los paramédicos en el campo.
Esperamos que el estudio piloto DOSE VF y la expansión de este ensayo a más sitios proporcionen pruebas de alto nivel en cuanto al beneficio potencial de las estrategias de desfibrilación alternativas para los pacientes que presentan una FV refractaria.
Todos los pacientes elegibles con FV refractaria (n = 128 hasta la fecha) en cuatro agencias del SEM participantes se han inscrito, y los Paramédicos han aplicado con éxito tanto el cambio de vector como la DSED sin problemas reportados.
Hemos demostrado que nuestro protocolo es factible y bien aceptado por los Paramédicos en el campo. Esperamos que el estudio piloto DOSE VF y la expansión de este ensayo a más sitios proporcionen pruebas de alto nivel en cuanto al beneficio potencial de las estrategias de desfibrilación alternativas para los pacientes que presentan una FV refractaria.
EN CLONCLUSIÓN, DSED sigue siendo una posible terapia alternativa existente para los pacientes que presentan FV refractaria. Aunque existe controversia en cuanto al mecanismo del efecto, los ensayos de investigación de alta calidad actuales y futuros pueden aclarar la efectividad pragmática de la DSED para la FV refractaria en el contexto prehospitalario.
REFERENCIAS
1. Hoch DH, Batsford WP, Greenberg SM, et al. Choques externos secuenciales dobles para fibrilación ventricular refractaria. Am Coll Cardiol 1994: 23: 1141-5.
2. Marrouche NF, Bardy GH, Frielitz HJ, Gunther J, Brachmann J. Enfoque de almohadillas cuádruples para la cardioversión externa de la fibrilación auricular. Estimulación Clin Electrophysiol. 2001; 24: 1321-1324.
3. Chang MS, Inouye H, Kallok MJ, Zipes DP. Las descargas secuenciales dobles y triples reducen el umbral de fibrilación ventricular en cerdos con y sin infarto de miocardio. J Am Coll Cardiol 1986; 8: 1393-1405.
4. Jones DL, Klein GJ, Guiraudon, Sharma AD. Desfibrilación secuencial por pulsos en humanos: desfibrilación secuencial ortogonal por pulsos con electrodos epicárdicos. J Am Coll Cardiol 1988; 11: 590-596.
5. Pagan-Carlo LA, Allan JJ, Spencer KT, Birkett CL, Myers R, Kerber RE. Formas de onda de choque multipulso superpuestas circundantes para desfibrilación transtorácica. J Am Coll Cardiol 1998; 32 (7): 2065-71.
6. Kerber RE, Martins B, Kienzle MG, et al. Energía, corriente y éxito en desfibrilación y cardioversión: estudios clínicos que utilizan un método automatizado de ajuste de energía basado en impedancia. Circulación 1988; 77: 1038-46.
7. Gerstein NS, Shah MB, Jorgensen KM. Uso simultáneo de dos desfibriladores para la conversión de fibrilación ventricular refractaria. Cardiothorac Vasc Anesth 2015; 29: 421-4.
8. Alaeddini J, Feng Z, Feghali G, Dufrene S, Davison NH, Abi-Samra FM. Las cardioversiones directas externas dobles repetidas que utilizan dos descargas simultáneas de 360 J para la fibrilación auricular refractaria son seguras y eficaces. Estimulación Clin Electrophysiol. 2005; 28: 3–7.
9. Cabanas JG, Myers J, Williams G, De Maio V, Bachman MW. Desfibrilación externa secuencial doble en fibrilación ventricular refractaria extrahospitalaria: un informe de casos frecuentes. Prehosp Emerg Care 2015; 19: 126-30.
10. Ross EM, Redman TT, Harper SA, Mapp JG, Wampler DA, Miramontes DA. Desfibrilación dual en el paro cardíaco extrahospitalario: un análisis de cohorte retrospectivo. Reanimación 2016; 106: 14-17.
11. Beck LR, Ostermayer DG, Ponce JN, Srinivasan S, Wang HE. Efectividad de la desfibrilación secuencial dual prehospitalaria para la fibrilación ventricular refractaria y la parada cardíaca por taquicardia ventricular. Atención de emergencia prehospitalaria. DOI: 10.1080 / 10903127.2019.1584256
12. Lybeck AM, Moy HP, Tan DK. Desfibrilación secuencial doble para fibrilación ventricular refractaria: reporte de un caso. Prehosp Emerg Care 2015; 19: 554-7.
13. Johnston M, Cheskes S, Ross G, Verbeek PR. Desfibrilación externa secuencial doble y supervivencia a paro cardíaco extrahospitalario: reporte de un caso. Prehosp Emerg Care 2016: 1-5.
14. Leacock BW. Desfibriladores dobles simultáneos para fibrilación ventricular refractaria. Emerg Med 2014; 46: 472-4.
15. Cortez E, Krebs W, Davis J, Keseg DP, Panchal AR. Uso de desfibrilación externa secuencial doble para la fibrilación ventricular refractaria durante un paro cardíaco extrahospitalario. Reanimación 2016; 108: 82-86.
16. Bartos JA, Carlson K, Carlson C, Raveendran G, John R, Aufderheide TP, Yannopoulos D. Sobrevivir al paro cardíaco por fibrilación ventricular extrahospitalaria refractaria:
Manejo de cuidados intensivos y oxigenación por membrana extracorpórea. Reanimación 132 (2018) 47-55.
17. Bartos JA, Carlson C, Grunau B, Duval S, Raveendran G, John R, Aufderheide TP, Yannopoulos D. Progressive Metabolic Derangement during Prolonged Resuscitation for Refractory VT / VF Cardiac Arrest and the Relationship to Neurologically Intact Survival with Extracorporeus Cardiopulary . Circulación. 2018; 138: A19.
18. Mittal et al. Comparación de una nueva forma de onda bifásica rectilínea con una forma de onda monofásica de onda sinusoidal amortiguada para la desfibrilación ventricular transtorácica
19. Directrices de 2005 de la American Heart Association para reanimación cardiopulmonar y atención cardiovascular de emergencia, parte 3: desfibrilación Circulación. 2005; 112: III-17 – III-24. J Am Coll Cardiol 1999; 34: 1595–601.
20. Delorenzo A, Nehme Z, Yates J, Bernard S, Smith K. Desfibrilación externa secuencial doble para fibrilación ventricular refractaria Paro cardíaco extrahospitalario: una revisión sistemática y un metanálisis. Reanimación 135 (2019) 124-129.
21. Johnson EE, Alforness CA, Wolf PD, Smith WM, Ideker RE. Efecto de la separación de pulsos entre dos descargas bifásicas administradas sobre diferentes configuraciones de cables sobre la eficacia de la desfibrilación ventricular. Circulación 1992; 85: 2267-74.
22. Gerstein NS, McLean R, Stecker EC, Schulman PM. Daño del desfibrilador externo asociado con un intento de cardioversión sincronizada de dosis dual. Anales de EM. 2018; 71: 109-112.
23. Comunicación. Physio-Control, Inc.
24. Marrouche NF, Bardy GH, Frielitz HJ, Gunther J, Brachmann J. Enfoque de almohadillas cuádruples para la cardioversión externa de la fibrilación auricular. Estimulación Clin Electrophysiol. 2001; 24: 1321-1324.
25. Davis M, Schappert A, Van Aarsen K, Loosley J, McLeod SL, Cheskes S. Un análisis descriptivo del cambio del vector de desfibrilación para la fibrilación ventricular refractaria prehospitalaria. CJEM. 2018; 20 (S1): S67.
- LUCAS CPR and ResQPod impedance threshold device
- Multiple defibrillations
- Amiodarone
- Magnesium
- Lidocaine
- Esmolol
- Hoch et al. “Double sequential external shocks for refractory ventricular fibrillation.” Journal of the American College of Cardiology. April 1994. 23(5): 1141.
- Xie et all. High-Energy Defibrillation Increases the Severity of Postresuscitation Myocardial Dysfunction. Circulation 1997;96:683.
- Walcott et al. Comparison of low-energy versus high-energy biphasic defibrillation shocks following prolonged ventricular fibrillation. Prehospital Emergency Care 2010;14(1):62.
- Geddes et al. The increased efficacy of high-energy defibrillation. Medical and biological engineering 1976;14(3):330.
Desfibriladores Externo-Automáticos DEA by FDA de los EUA
https://emssolutionsint.blogspot.com/2021/08/desfibriladores-externo-automaticos-dea.html
Utilizar un Desfibrilador Externo-Automático DEA en un paciente con Marcapasos Implantado https://emssolutionsint.blogspot.com/2023/12/utilizar-un-desfibrilador-externo.html
SEÑAL UNIVERSAL PARA DESFIBRILADORES EXTERNO-AUTOMATICOS, DEA, AED, DESA, ILCOR
https://emssolutionsint.blogspot.com/2010/12/senal-universal-para-desfibriladores.html
Aspectos destacados de las guías de la american heart association del 2020 para RCP y ACE
https://emssolutionsint.blogspot.com/2020/10/aspectos-destacados-de-las-guias-de-la.html
REPUBLICA DOMINICANA CARDIOPROTEGIDA Estimado Desfibriladores Externo Automáticos AED, DESA, AED por país por cada 10,000 habitantes. "REPUBLICA DOMINICANA CARDIOPROTEGIDA / RCP-DEA "
https://emssolutionsint.blogspot.com/2012/03/republica-dominicana-cardioprotegida.html
Nueva Cadena de Supervivencia en RCP . Curva Drinker VIDEO
https://emssolutionsint.blogspot.com/2011/04/nueva-cadena-de-supervivencia-2010-215.html
Paro cardíaco súbito versus ataque cardíaco repentino/ Cardiac Arrest vs Hear Attack. by CardioSmart
https://emssolutionsint.blogspot.com/2023/06/sudden-cardiac-arrest-vs-hear-attack.html
PRIMER DESFIBRILADOR DEL BOLSILLO DEL MUNDO/ Smallest AED in the Market Fred Easyport
https://emssolutionsint.blogspot.com/2012/02/smallest-aed-in-market-fred-easyport.html
¿En qué consiste un desfibrilador? by Fundación Española del Corazón
https://emssolutionsint.blogspot.com/2023/08/en-que-consiste-un-desfibrilador-by.html
desfibrilación o cardioversión no sincronizada
https://emssolutionsint.blogspot.com/2023/07/desfibrilacion-o-cardioversion-no.html





No hay comentarios:
Publicar un comentario