Tourniquets in TCCC
JTS / CoTCCC
Tourniquets in TCCC Guidelines (Dec 2021)
Massive bleeding or uncontrolled hemorrhage is the leading cause of preventable death on the battlefield, and as a result it is the number one medical priority in the CUF phase of TCCC. Early control of severe hemorrhage is critical to survival. Injury to a major vessel can quickly lead to shock and death. Due to the hostile environment encountered during CUF, only life-threatening bleeding warrants intervention.
TCCC CUF
Basic Management Plan for Care Under Fire / Threat
1. Return fire and take cover.
2. Direct or expect casualty to remain engaged as a combatant if appropriate.
3. Direct casualty to move to cover and apply self-aid if able or when tactically feasible, move or drag casualty to cover.
4. Try to keep the casualty from sustaining additional wounds.
5. Casualties should be extracted from burning vehicles or buildings and moved to places of relative safety. Do what is necessary to stop the burning process.
6. Stop life-threatening external hemorrhage if tactically feasible:
Direct casualty to control hemorrhage by self-aid if able.
Use a CoTCCC-recommended limb tourniquet for hemorrhage that is anatomically amenable to tourniquet use.
Apply the limb tourniquet over the uniform clearly proximal to the bleeding site(s). If the site of the life-threatening bleeding is not readily apparent, place the tourniquet “high and tight” (as proximal as possible) on the injured limb and move the casualty to cover.
7. Airway management is generally best deferred until the Tactical Field Care phase.
TFC Massive Hemorrhage
a. Assess for unrecognized hemorrhage and control all sources of bleeding. If not already done, use a CoTCCC-recommended limb tourniquet to control life- threatening external hemorrhage that is anatomically amenable to tourniquet use or for any traumatic amputation. Apply directly to the skin 2-3 inches above the bleeding site. If bleeding is not controlled with the first tourniquet, apply a second tourniquet side-by-side with the first.
b. For compressible (external) hemorrhage not amenable to limb tourniquet use or as an adjunct to tourniquet removal, use Combat Gauze as the CoTCCC hemostatic dressing of choice.
Alternative hemostatic adjuncts:
Celox Gauze or
ChitoGauze or
XStat (Best for deep, narrow-tract junctional wounds)
iTClamp (may be used alone or in conjunction with hemostatic dressing or XStat.
Hemostatic dressings should be applied with at least 3 minutes of direct pressure (optional for XStat). Each dressing works differently, so if one fails to control bleeding, it may be removed and a fresh dressing of the same type or a different type applied. (Note: XStat is not to be removed in the field, but additional XStat, other hemostatic adjuncts, or trauma dressings may be applied over it.)
If the bleeding site is amenable to use of a junctional tourniquet, immediately apply a junctional tourniquet. Do not delay in the application of the junctional tourniquet once it is ready for use. Apply hemostatic dressings with direct pressure if a junctional tourniquet is not available or while the junctional tourniquet is being readied for use.
TFC Circulation - Bleeding
a. Bleeding
Reassess prior tourniquet application. Expose the wound and determine if a tourniquet is needed. If it is needed, replace any limb tourniquet placed over the uniform with one applied directly to the skin 2-3 inches above the bleeding site. Ensure that bleeding is stopped. If there is no traumatic amputation, a distal pulse should be checked. If bleeding persists or a distal pulse is still present, consider additional tightening of the tourniquet or the use of a second tourniquet side-by-side with the first to eliminate both bleeding and the distal pulse. If the reassessment determines that the prior tourniquet was not needed, then remove the tourniquet and note time of removal on the TCCC Casualty Card.
Limb tourniquets and junctional tourniquets should be converted to hemostatic or pressure dressings as soon as possible if three criteria are met: the casualty is not in shock; it is possible to monitor the wound closely for bleeding; and the tourniquet is not being used to control bleeding from an amputated extremity. Every effort should be made to convert tourniquets in less than 2 hours if bleeding can be controlled with other means. Do not remove a tourniquet that has been in place more than 6 hours unless close monitoring and lab capability are available.
Expose and clearly mark all tourniquets with the time of tourniquet application. Note tourniquets applied and time of application; time of re- application; time of conversion; and time of removal on the TCCC Casualty Card. Use a permanent marker to mark on the tourniquet and the casualty card.
Life-Threatening Bleeding
JTS / CoTCCC
Tourniquets in TCCC Guidelines (Dec 2021)
Massive bleeding or uncontrolled hemorrhage is the leading cause of preventable death on the battlefield, and as a result it is the number one medical priority in the CUF phase of TCCC. Early control of severe hemorrhage is critical to survival. Injury to a major vessel can quickly lead to shock and death. Due to the hostile environment encountered during CUF, only life-threatening bleeding warrants intervention.
TCCC CUF
Basic Management Plan for Care Under Fire / Threat
1. Return fire and take cover.
2. Direct or expect casualty to remain engaged as a combatant if appropriate.
3. Direct casualty to move to cover and apply self-aid if able or when tactically feasible, move or drag casualty to cover.
4. Try to keep the casualty from sustaining additional wounds.
5. Casualties should be extracted from burning vehicles or buildings and moved to places of relative safety. Do what is necessary to stop the burning process.
6. Stop life-threatening external hemorrhage if tactically feasible:
Direct casualty to control hemorrhage by self-aid if able.
Use a CoTCCC-recommended limb tourniquet for hemorrhage that is anatomically amenable to tourniquet use.
Apply the limb tourniquet over the uniform clearly proximal to the bleeding site(s). If the site of the life-threatening bleeding is not readily apparent, place the tourniquet “high and tight” (as proximal as possible) on the injured limb and move the casualty to cover.
7. Airway management is generally best deferred until the Tactical Field Care phase.
TFC Massive Hemorrhage
a. Assess for unrecognized hemorrhage and control all sources of bleeding. If not already done, use a CoTCCC-recommended limb tourniquet to control life- threatening external hemorrhage that is anatomically amenable to tourniquet use or for any traumatic amputation. Apply directly to the skin 2-3 inches above the bleeding site. If bleeding is not controlled with the first tourniquet, apply a second tourniquet side-by-side with the first.
b. For compressible (external) hemorrhage not amenable to limb tourniquet use or as an adjunct to tourniquet removal, use Combat Gauze as the CoTCCC hemostatic dressing of choice.
Alternative hemostatic adjuncts:
Celox Gauze or
ChitoGauze or
XStat (Best for deep, narrow-tract junctional wounds)
iTClamp (may be used alone or in conjunction with hemostatic dressing or XStat.
Hemostatic dressings should be applied with at least 3 minutes of direct pressure (optional for XStat). Each dressing works differently, so if one fails to control bleeding, it may be removed and a fresh dressing of the same type or a different type applied. (Note: XStat is not to be removed in the field, but additional XStat, other hemostatic adjuncts, or trauma dressings may be applied over it.)
If the bleeding site is amenable to use of a junctional tourniquet, immediately apply a junctional tourniquet. Do not delay in the application of the junctional tourniquet once it is ready for use. Apply hemostatic dressings with direct pressure if a junctional tourniquet is not available or while the junctional tourniquet is being readied for use.
TFC Circulation - Bleeding
a. Bleeding
Reassess prior tourniquet application. Expose the wound and determine if a tourniquet is needed. If it is needed, replace any limb tourniquet placed over the uniform with one applied directly to the skin 2-3 inches above the bleeding site. Ensure that bleeding is stopped. If there is no traumatic amputation, a distal pulse should be checked. If bleeding persists or a distal pulse is still present, consider additional tightening of the tourniquet or the use of a second tourniquet side-by-side with the first to eliminate both bleeding and the distal pulse. If the reassessment determines that the prior tourniquet was not needed, then remove the tourniquet and note time of removal on the TCCC Casualty Card.
Limb tourniquets and junctional tourniquets should be converted to hemostatic or pressure dressings as soon as possible if three criteria are met: the casualty is not in shock; it is possible to monitor the wound closely for bleeding; and the tourniquet is not being used to control bleeding from an amputated extremity. Every effort should be made to convert tourniquets in less than 2 hours if bleeding can be controlled with other means. Do not remove a tourniquet that has been in place more than 6 hours unless close monitoring and lab capability are available.
Expose and clearly mark all tourniquets with the time of tourniquet application. Note tourniquets applied and time of application; time of re- application; time of conversion; and time of removal on the TCCC Casualty Card. Use a permanent marker to mark on the tourniquet and the casualty card.
Life-Threatening Bleeding
A tourniquet cuts off the flow of blood to the arm or leg past the application site and is the best method to control massive bleeding from an arm or a leg.
Tourniquets can be self-applied or applied to a casualty using either a one-handed or two-handed technique. Self-application of a tourniquet might also save your life.
A tourniquet will hurt when applied correctly, because it must be tight enough to stop the blood flow.
Remember to tell the casualty that pain is expected and is an indicator that the tourniquet is being applied properly (tight enough).
The application of a tourniquet to a massive bleed is time-sensitive! The tourniquet should be applied to stop bleeding within 1 minute and be fully secured within 3 minutes. A casualty with massive bleeding that is not controlled can die within 3 minutes!!!
Tourniquets can be self-applied or applied to a casualty using either a one-handed or two-handed technique. Self-application of a tourniquet might also save your life.
A tourniquet will hurt when applied correctly, because it must be tight enough to stop the blood flow.
Remember to tell the casualty that pain is expected and is an indicator that the tourniquet is being applied properly (tight enough).
The application of a tourniquet to a massive bleed is time-sensitive! The tourniquet should be applied to stop bleeding within 1 minute and be fully secured within 3 minutes. A casualty with massive bleeding that is not controlled can die within 3 minutes!!!
Tourniquet REASSESSMENT
All Tourniquets should be reassessed frequently
Previously applied tourniquets should be assessed for effectiveness (bleeding has been stopped and distal pulses are absent).
If the tourniquet is not effective, tighten the tourniquet and/or apply a second tourniquet side-by-side and proximal to the first one.
Assess for unrecognized hemorrhage and control all sources of bleeding. If not already done, use a CoTCCC-recommended limb tourniquet to control life-threatening external hemorrhage that is anatomically amenable to tourniquet use or for any traumatic amputation. Apply directly to the skin 2-3 inches above the bleeding site. If bleeding is not controlled with the first tourniquet, apply a second tourniquet side-by-side with the first.
If a tourniquet was applied and not needed, the tourniquet should be converted as soon as possible within 2 hours of application and no longer than 6 hours after application.
All Tourniquets should be reassessed frequently
Previously applied tourniquets should be assessed for effectiveness (bleeding has been stopped and distal pulses are absent).
If the tourniquet is not effective, tighten the tourniquet and/or apply a second tourniquet side-by-side and proximal to the first one.
Assess for unrecognized hemorrhage and control all sources of bleeding. If not already done, use a CoTCCC-recommended limb tourniquet to control life-threatening external hemorrhage that is anatomically amenable to tourniquet use or for any traumatic amputation. Apply directly to the skin 2-3 inches above the bleeding site. If bleeding is not controlled with the first tourniquet, apply a second tourniquet side-by-side with the first.
If a tourniquet was applied and not needed, the tourniquet should be converted as soon as possible within 2 hours of application and no longer than 6 hours after application.
Tourniquet Assessment
After reassessing bleeding control, if appropriate, the next step is to expose any wounds, if that has not already been accomplished. Wound exposure should be accomplished using trauma shears rather than an unguarded blade to prevent further injury to the extremity.
The objective of this is to determine if the bleeding from the wound might be controlled without a tourniquet and/or to assess whether a tourniquet might be applied closer to the wound to preserve as much viable tissue as possible.
There is no precise set of parameters that will universally help make the determination of whether a tourniquet is necessary, but typical injuries that will continue to require a tourniquet include some obvious injuries like amputations and deep wounds that resulted in severed arteries, whereas more superficial injuries not involving the arteries may be more easily controlled. However, sometimes the extent of the wound isn’t clearly known just based on the external view of the wound.
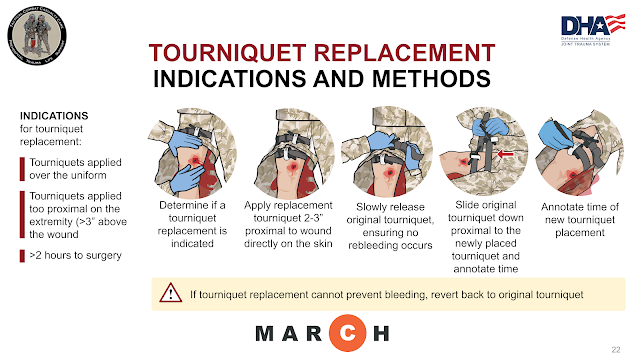
Tourniquet REPLACEMENT
After reassessing bleeding control, if appropriate, the next step is to expose any wounds, if that has not already been accomplished. Wound exposure should be accomplished using trauma shears rather than an unguarded blade to prevent further injury to the extremity.
The objective of this is to determine if the bleeding from the wound might be controlled without a tourniquet and/or to assess whether a tourniquet might be applied closer to the wound to preserve as much viable tissue as possible.
There is no precise set of parameters that will universally help make the determination of whether a tourniquet is necessary, but typical injuries that will continue to require a tourniquet include some obvious injuries like amputations and deep wounds that resulted in severed arteries, whereas more superficial injuries not involving the arteries may be more easily controlled. However, sometimes the extent of the wound isn’t clearly known just based on the external view of the wound.
Tourniquet REPLACEMENT
Tourniquet Replacement
In massive hemorrhage you learned that tourniquets should be applied more deliberately in the tactical field care setting, to maximize effectiveness and minimize the amount of healthy tissue that might be impacted by a tourniquet placed too high on the limb.
If a tourniquet is, in fact, necessary, replace high and tight tourniquets or tourniquets applied over the clothing with more deliberate tourniquets.
This is done by placing a replacement tourniquet directly on the skin, 2-3 inches above the wound and tightening it. Then, slowly release the original tourniquet over one minute, while monitoring the casualty for signs of recurrent bleeding or resumption of a distal pulse. Slide originally placed tourniquet(s) down, but leave in place proximal to the newly placed tourniquet. In cases of recurrent bleeding or pulses, the original tourniquet can be retightened and the replacement tourniquet can be tightened further, or repositioned and tightened further.
Afterwards, the original tourniquet is slowly released again to confirm bleeding control. It may require a second tourniquet be placed side-by-side with the replacement tourniquet, as well.
Occasionally an attempt to replace a tourniquet will not be successful, and reverting back to the prior tourniquet location may be needed.
If the initial tourniquet remains tightened in its original position, there is a risk of a compartment syndrome developing between the two tourniquets. But rather than removing the original tourniquet completely, it can be slid down the extremity and positioned just proximal to the replacement tourniquet, but only partially tightened by having the slack of the tourniquet removed and the strap secured to prevent it from catching or being in the way during casualty assessments or movements.
Tourniquet CONVERSION
In massive hemorrhage you learned that tourniquets should be applied more deliberately in the tactical field care setting, to maximize effectiveness and minimize the amount of healthy tissue that might be impacted by a tourniquet placed too high on the limb.
If a tourniquet is, in fact, necessary, replace high and tight tourniquets or tourniquets applied over the clothing with more deliberate tourniquets.
This is done by placing a replacement tourniquet directly on the skin, 2-3 inches above the wound and tightening it. Then, slowly release the original tourniquet over one minute, while monitoring the casualty for signs of recurrent bleeding or resumption of a distal pulse. Slide originally placed tourniquet(s) down, but leave in place proximal to the newly placed tourniquet. In cases of recurrent bleeding or pulses, the original tourniquet can be retightened and the replacement tourniquet can be tightened further, or repositioned and tightened further.
Afterwards, the original tourniquet is slowly released again to confirm bleeding control. It may require a second tourniquet be placed side-by-side with the replacement tourniquet, as well.
Occasionally an attempt to replace a tourniquet will not be successful, and reverting back to the prior tourniquet location may be needed.
If the initial tourniquet remains tightened in its original position, there is a risk of a compartment syndrome developing between the two tourniquets. But rather than removing the original tourniquet completely, it can be slid down the extremity and positioned just proximal to the replacement tourniquet, but only partially tightened by having the slack of the tourniquet removed and the strap secured to prevent it from catching or being in the way during casualty assessments or movements.
Tourniquet CONVERSION
Tourniquet Conversion
Every effort should be made to convert tourniquets in less than 2 hours if bleeding can be controlled by other means, unless the casualty is in shock, you cannot closely monitor the wound for re-bleeding, or there has been an amputation; however, do not attempt tourniquet conversion if the tourniquet has been on for six or more hours. Also, consider leaving the tourniquet in place if the tactical or medical considerations make transition to other hemorrhage control methods inadvisable.
While the original tourniquet is still in place controlling the bleeding, pack the wound with hemostatic gauze, if available, and hold pressure for three minutes. Then apply a pressure bandage over the dressing, maintaining pressure. Afterwards, slowly release the tourniquet (over at least one minute) while closely observing for bleeding. If the wound packing and pressure bandage do not control the bleeding, retighten the tourniquet or follow the steps to replace the tourniquet if it is above the clothing, like a high and tight tourniquet. In cases where the conversion has failed, it is appropriate to try again within the next two hours, as long as it hasn’t been more than six hours since the original tourniquet was applied.
If the conversion is successful, loosen the tourniquet and move it down to just above the pressure dressing, loose but with the no slack in the strap, in case it is needed later, and annotate the time of tourniquet removal on the DD Form 1380, TCCC Casualty Card. Periodically reassess the wound for recurrent bleeding and reassess after any casualty movements.
Tourniquet PRINCIPLES
CoTCCC Recommended Tourniquets
Combat Application Tourniquet (CAT) Gen 7
NSN: 6515-01-521-7976DLA Nomenclature: Tourniquet Nonpneumatic Combat Application One-Handed 37.5" LG 1
Combat Application Tourniquet (CAT) Gen 6
NSN: Use of CAT Generation 6 is acceptable until life-cycle replacements to gen 7.
DLA Nomenclature: Tourniquet Nonpneumatic Combat Application One-Handed 37.5" LG 1
Ratcheting Medical Tourniquet -Tactical (RMT-T)
NSN: 6515-01-527-3841
DLA Nomenclature: Tourniquet, One Handed Burke Device Tactical
NOTE: The RMT Civilian models are not CoTCCC-recommended for military use.
SAM Extremity Tourniquet (SAM-XT)
NSN: 6515-01-670-2240
DLA Nomenclature: Tourniquet Nonpneumatic 25S
SOF Tactical Tourniquet – Wide (SOFTT-W)
NSN: 6515-01-587-9943
DLA Nomenclature: Tourniquet Nonpneumatic Nylon Strap 1.5” Wide Nylon Strap for BR
NOTE: The original 1” SOFTT is removed from the CoTCCC Recommendations.
Tactical Mechanical Tourniquet (TMT)
NSN: 6515-01-656-6191
DLA Nomenclature: Tourniquet Nonpneumatic Tactical Mechanical Tourniquet
TX2” Tourniquet (TX2)
NSN: 6515-01-667-6027
DLA Nomenclature: Tourniquet Nonpneumatic TX2 Ratcheting One-Hand Coyote
TX3” Tourniquet (TX3)
NSN: 6515-01-667-6208
DLA Nomenclature: Tourniquet Nonpneumatic TX2 Ratcheting OD Green
Emergency & Military Tourniquet (EMT)
NSN: 6515-01-580-1645DLA Nomenclature: Tourniquet Pneumatic Single-hand application fits upper and lower
NOTE: Not recommended for JFAK, but considered for medics, evacuation platforms and Role I/II/III teams primarily for TQ-replacement, conversion, or prolonged application.
Tactical Pneumatic Tourniquet 2” (TPT2)
NSN: 6515-01-656-4831
DLA Nomenclature: Tourniquet Pneumatic Slide Fastener
NOTE: Not recommended for JFAK, but considered for medics, evacuation platforms and Role I/II/III teams primarily for TQ-replacement, conversion, or prolonged application.
Tourniquets
Death from extremity hemorrhage can be prevented by aggressive use of tourniquets unless the site of bleeding is too proximal on the extremity to apply a tourniquet. Because of their effectiveness at hemorrhage control, the speed with which they can be applied, and the lack of a requirement to hold sustained direct pressure on the bleeding site, tourniquets are the best option for temporary control of life-threatening extremity hemorrhage in the tactical environment. Tourniquets are far more effective at saving lives when applied before the casualty has gone into hemorrhagic shock.
Past concerns about ischemic damage to extremities from brief periods of tourniquet use have proven to be unfounded when tourniquets are used appropriately and for short periods of time. Tourniquets have been found to be safe if left on for less than 2 hours. Prolonged (> 6 hours) use of a tourniquet can potentially result in the loss of a limb, but there were no reports of limb loss in U.S. casualties due to tourniquet ischemia in a large review of tourniquet use in Iraq and Afghanistan.
Every combatant on the battlefield should be able to apply a tourniquet to his or her own bleeding extremity and to the arm or leg of any other unit member who requires it. Hemorrhage control by nonmedical personnel has been a key element in reducing preventable deaths on the battlefield.43 When applied, tourniquets should be placed over the uniform just proximal to the site of the severe bleeding. If the bleeding site cannot be precisely located due to darkness or the need for expedited application during an engagement with hostile forces, the tourniquet should be applied as proximally on the extremity as feasible. If bleeding does not stop after the first tourniquet has been tightened, a second tourniquet should be applied adjacent to the first.
Tourniquets should never be placed directly over a joint. They should also never be placed over a holster or a pocket containing bulky objects that would make tightening the tourniquet more difficult or make tourniquet application more painful for the casualty. During Care Under Fire, tourniquets should be tightened as necessary to stop the bleeding from the distal injury. Having the tourniquet placed over the uniform is not ideal, but Care Under Fire is not the right time to expose the wound for a thorough examination. Rather, the bleeding should be stopped, and both the casualty and the care provider should move to cover as quickly as possible. Once time permits in the Tactical Field Care phase, the wound should be exposed and reevaluated, and a replacement tourniquet should be applied directly to the casualty’s skin.
The time of tourniquet application should always be documented. This has customarily been accomplished by writing the letter “T” on the casualty’s forehead along with the time. This should be done with an indelible ink marker to ensure that this important information does not wash or wipe off. Either on the involved extremity or a piece of tape applied to the casualty’s chest is an alternative location for noting tourniquet application time. The information should also be recorded on the individual’s TCCC Casualty Card. If the casualty has multiple tourniquets with significantly different times of application, this should be noted clearly in the first responder care documentation. All manufactured tourniquets are designed for a single use. A separate group of tourniquets should be used for training, and training tourniquets should not subsequently be issued to individuals for use in combat. Many military units have evolved to a single-tour, single-use policy for tourniquets. Direct pressure and compression dressings are less desirable than tourniquets during Care Under Fire because the need for direct pressure may result in lethal delays in getting the casualty and the rescuer to cover. Furthermore, these interventions provide less definitive control of life-threatening extremity hemorrhage, especially while the casualty is being moved.
A final note about tourniquets: They should be protected from exposure to the elements during combat deployments. In 2013, Weppner and colleagues studied tourniquets that were carried by Marine Corps personnel on their plate carriers during a deployment, comparing them to tourniquets that were carried inside individual first aid kits (IFAKs).47 Of the plate carrier-exposed tourniquets, (12%) broke when tested as opposed to none among those carried in IFAKs.
References
Shackelford SA, Butler FK Jr, Kragh JF Jr, et al. Optimizing the use of limb tourniquets in Tactical Combat Casualty Care: TCCC guidelines change 14-02. J Spec Oper Med. 2015;15:17-31.
Drew B, Bird D, Matteucci M, Keenan S. Tourniquet Conversion: A Recommended Approach in the Prolonged Field Care Setting. J Spec Oper Med. 2015 Fall;15(3):81-85.
Montgomery HR, Hammesfahr R, Fisher AD, Cain JS, Greydanus DJ, Butler FK Jr, Goolsby C, Eastman AL. 2019 Recommended Limb Tourniquets in Tactical Combat Casualty Care. J Spec Oper Med. 2019 Winter;19(4):27-50.
Kragh JF, Walters TJ, Baer DG, et al. Practical use of emergency tourniquets to stop bleeding in major limb trauma. J Trauma. 2008;64(Suppl 2):S38-S50. doi:10.1097/TA.0b013e31816086b1.
Kragh JF, Walters TJ, Baer DG, et al. Survival with emergency tourniquet use to stop bleeding in major limb trauma. Ann Surg. 2009;249(1):1-7. doi:10.1097/SLA.0b013e31818842ba.
Lakstein D, Blumenfeld A, Sokolov T, et al. Tourniquets for hemorrhage control on the battlefield: a 4-year accumulated experience. J Trauma. 2003;54(Suppl 5):S221-225.
Butler FK, Holcomb JB, Giebner SG, McSwain NE, Bagian J. Tactical Combat Casualty Care 2007: evolving concepts and battlefield experience. Mil Med. 2007;172(Suppl 11):1-19.
Butler FK. The US military experience with tourniquets and hemostatic dressings in the Afghanistan and Iraq conflicts. Bull Am College Surg. 2015;100(Sept Suppl):60-65.
Weppner J, Lang M, Sunday R, Debiasse N. Efficacy of tourniquets exposed to the Afghanistan combat environment stored in Individual First Aid Kits versus on the exterior of plate carriers. Mil Med. 2013;178:334-337.
Carey ME. Analysis of wounds incurred by US Army Seventh Corps personnel treated in corps hospitals during Operation Desert Storm, February 20 to March 10, 1991. J Trauma. 1996;40(Suppl 3):S165-S169.
Maughon JS. An inquiry into the nature of wounds resultingin killed in action in Vietnam. Mil Med. 1970;135(1):8-13.
Butler FK, Hagmann J, Butler EG. Tactical combat casualtycare in special operations. Mil Med. 1996;161(Suppl):3-16.
Por favor compartir nuestras REDES SOCIALES @DrRamonReyesMD, así podremos llegar a mas personas y estos se beneficiarán de la disponibilidad de estos documentos, pdf, e-book, gratuitos y legales..
Grupo Biblioteca/PDFs gratis en Facebookhttps://www.facebook.com/
Facebook
Pinterest
Twitter
Blog
Gracias a todos el Canal somos más de 1000 participantes en WhatsApp. Recordar este es un canal y sirve de enlace para entrar a los tres grupos; TACMED, TRAUMA y Científico. ahí es que se puede interactuar y publicar. Si le molestan las notificaciones, solo tiene que silenciarse y así se beneficia de la información y la puede revisar cuando usted así lo disponga sin el molesto sonido de dichas actualizaciones, Gracias a todos Dr. Ramon Reyes, MD Enlace al
Enlace a TACMED en WhatsApp https://chat.
Enlace a TRAUMA en WhatsApp https://chat.
Enlace a Científico https://chat.
TELEGRAM Emergencias https://t.me/+sF_-
TELEGRAM TACMED https://t.me/CIAMTO
Grupo Biblioteca/PDFs gratis en Facebook
https://www.facebook.com/
Facebook
Pinterest
Twitter
Blog
Gracias a todos el Canal somos más de 1000 participantes en WhatsApp. Recordar este es un canal y sirve de enlace para entrar a los tres grupos; TACMED, TRAUMA y Científico. ahí es que se puede interactuar y publicar. Si le molestan las notificaciones, solo tiene que silenciarse y así se beneficia de la información y la puede revisar cuando usted así lo disponga sin el molesto sonido de dichas actualizaciones, Gracias a todos Dr. Ramon Reyes, MD Enlace al
Enlace a TACMED en WhatsApp https://chat.
Enlace a TRAUMA en WhatsApp https://chat.
Enlace a Científico https://chat.
TELEGRAM Emergencias https://t.me/+sF_-
TELEGRAM TACMED https://t.me/CIAMTO
AVISO IMPORTANTE A NUESTROS USUARIOS
Este Blog va dirigido a profesionales de la salud y público en general EMS Solutions International garantiza, en la medida en que puede hacerlo, que los contenidos recomendados y comentados en el portal, lo son por profesionales de la salud. Del mismo modo, los comentarios y valoraciones que cada elemento de información recibe por el resto de usuarios registrados –profesionales y no profesionales-, garantiza la idoneidad y pertinencia de cada contenido.
Es pues, la propia comunidad de usuarios quien certifica la fiabilidad de cada uno de los elementos de información, a través de una tarea continua de refinamiento y valoración por parte de los usuarios.
Si usted encuentra información que considera errónea, le invitamos a hacer efectivo su registro para poder avisar al resto de usuarios y contribuir a la mejora de dicha información.
El objetivo del proyecto es proporcionar información sanitaria de calidad a los individuos, de forma que dicha educación repercuta positivamente en su estado de salud y el de su entorno. De ningún modo los contenidos recomendados en EMS Solutions International están destinados a reemplazar una consulta reglada con un profesional de la salud.



.png)








No comments:
Post a Comment